By 2025, Global HIV Stats Signal a Turning Tough, Yet Hopeful Trajectory as WHO Projects Climbing but Controlling Counts Across Regions
By 2025, Global HIV Stats Signal a Turning Tough, Yet Hopeful Trajectory as WHO Projects Climbing but Controlling Counts Across Regions
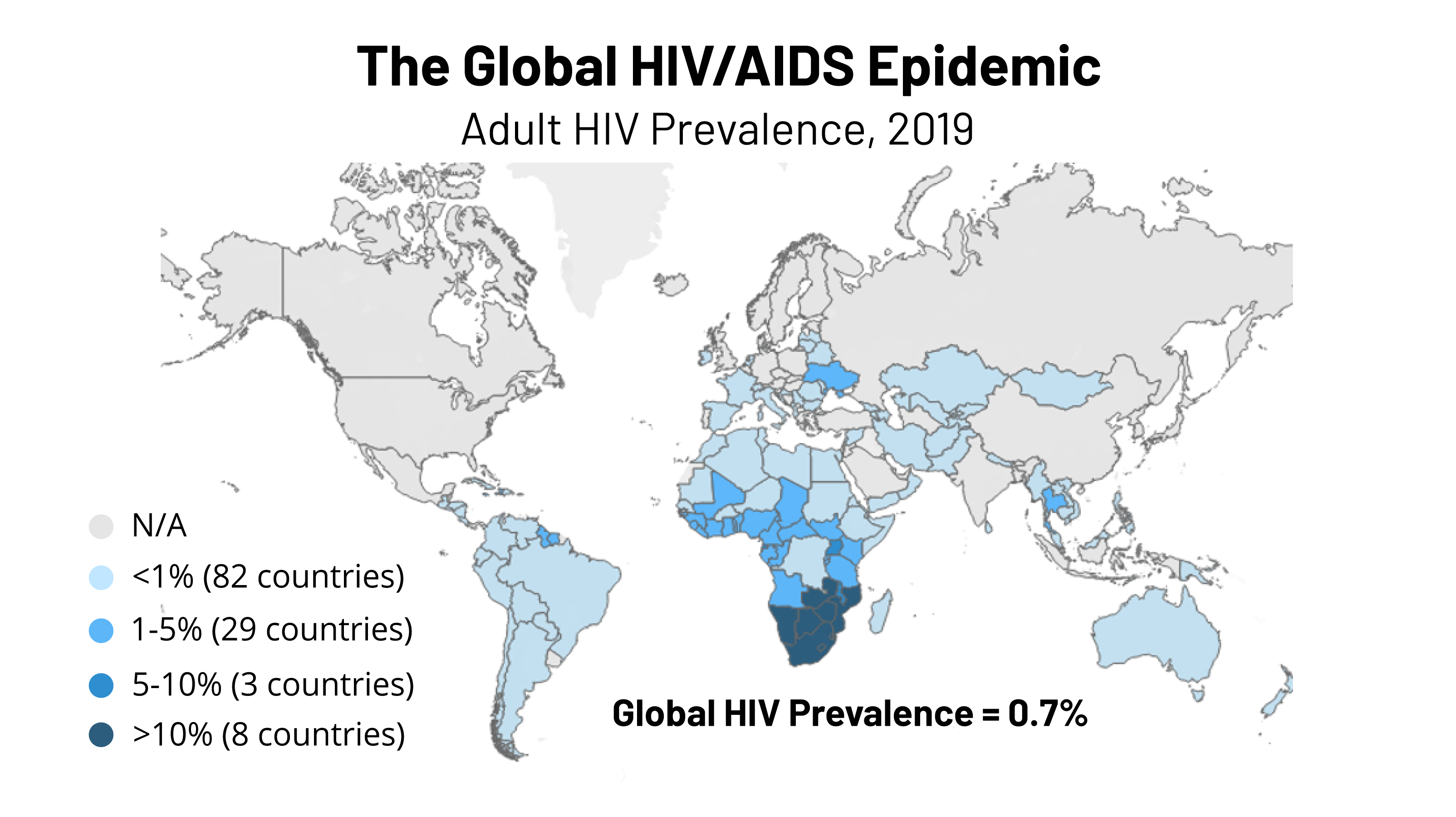
As the world edges toward 2025, HIV statistics reveal a complex and evolving landscape—one where progress remains uneven across WHO regions, but sustained global efforts are gradually stemming new infections and saving lives. The World Health Organization’s latest projections paint a nuanced picture: despite rising challenges, new HIV infections are expected to stabilize around 1.3 million annually, while AIDS-related deaths continue a steady decline, now hovering near 630,000—indicating a turning point in the fight against the epidemic. With targeted interventions accelerating in key areas, the next decade could redefine the global response to HIV, particularly as regional disparities shape where momentum builds and where gaps persist.
The WHO categorizes HIV burdens into six regions, each facing distinct epidemiological realities that influence the 2025 forecast. Sub-Saharan Africa, home to over two-thirds of the global HIV burden, remains the epicenter of the pandemic. According to the WHO’s Global HIV Report 2024, in 2025, new infections in this region are projected at approximately 1.2 million—slightly above current levels but poised to plateau, signaling a critical shift from decades of exponential growth.
“This plateau reflects the real impact of scaled-up testing, sustained antiretroviral treatment (ART) access, and prevention innovation,” stated Dr. Maria Van Kerkhove, Director of the WHO Health Emergencies Programme. “We’re no longer seeing unchecked progression, just a shifting baseline we must not cross.” Regionally, Eastern and Southern Africa—led by South Africa, Nigeria, and Egypt—are projected to account for nearly 40% of new infections by 2025.
These nations have made substantial strides through aggressive rollout of pre-exposure prophylaxis (PrEP), contact tracing, and clinic-based prevention services. South Africa, with an estimated 7.5 million people living with HIV, launched a national ART expansion campaign in 2023 that increased treatment coverage to 77% among those diagnosed, directly correlating with a projected 15% drop in new infections by 2025. “Community-led initiatives have been the game-changer here,” noted Dr.
Thuli Makama, a public health expert at the University of Cape Town. “When people trusted the health system—when testing, treatment, and prevention became local priorities—visibility and access improved dramatically.” In contrast, the Western Pacific region faces a different trajectory. Here, HIV incidence is stabilizing but remains stubbornly high in key populations such as men who have sex with men (MSM) in urban centers like Manila and Sydney, and people living in prison systems in Northern Asia.
The WHO projects new infections in this region to hold steady at around 130,000 annually, with Thailand and Indonesia leading prevention scaling efforts. “Sustained investment in harm reduction and stigma reduction is non-negotiable,” warned Dr. gaina Bailin, a regional advisor.
“Without addressing structural barriers—criminalization, criminalization, and exclusion—new infections in vulnerable groups will remain entrenched.” The Eastern Mediterranean region, including countries like Iran, Yemen, and Egypt, shows a mosaic of progress and fragility. While Iran has reduced new infections by nearly 40% since 2010 through aggressive PrEP rollout and widespread ART adherence, conflict zones such as Yemen see HIV dynamics severely disrupted by health system collapse. The WHO forecasts a new infection rate rise of 5–7% in fragile settings by 2025 due to interrupted services, underscoring how health security is inseparable from broader geopolitical stability.
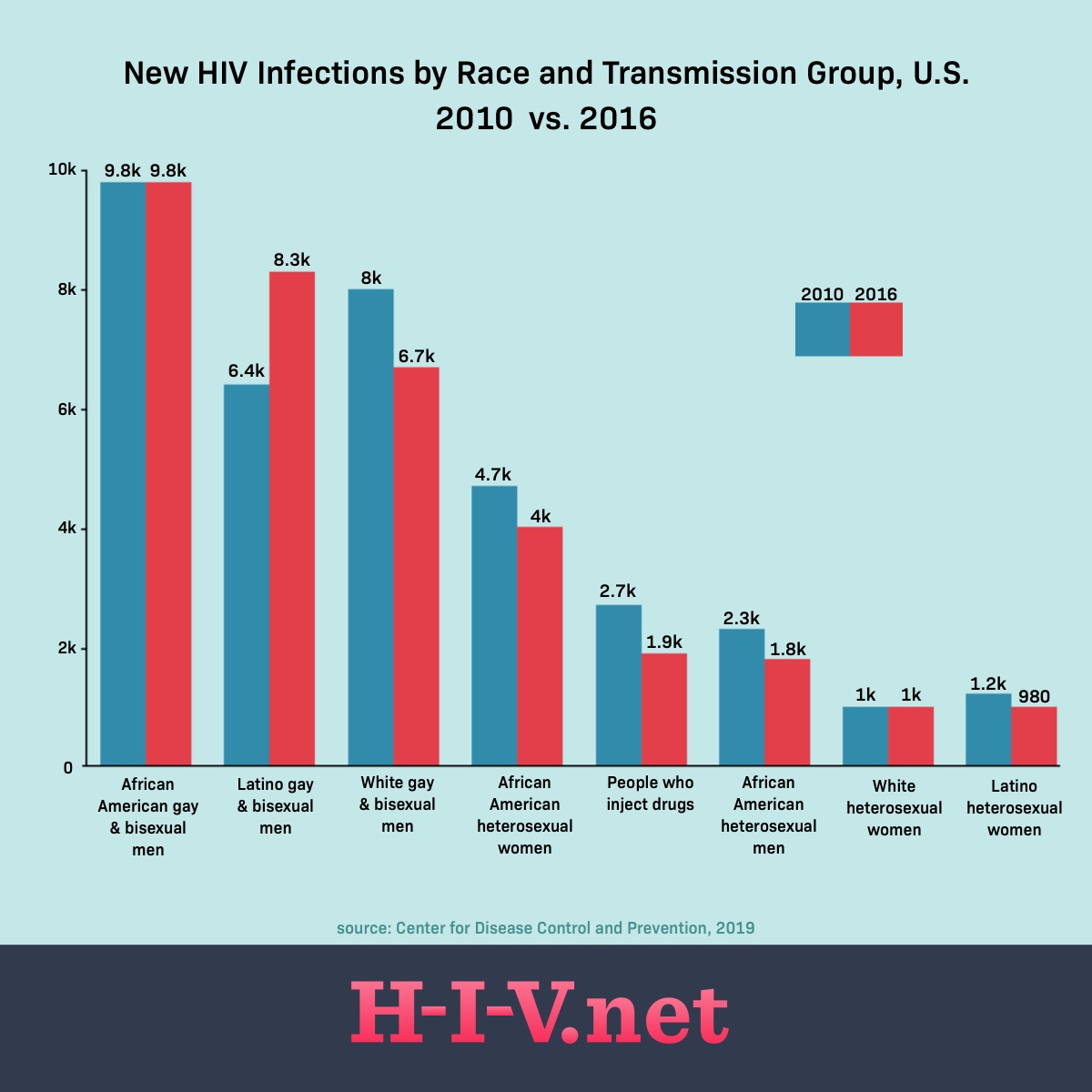
In the Americas, the focus remains on slowing advance in historically hard-hit areas such as the Caribbean and parts of Central America. Here, new infections hover around 160,000 annually, with Brazil and Mexico implementing robust digital outreach and self-testing programs that have reversed declines in testing uptake. Yet, marginalized communities—including transgender populations in Colombia and indigenous groups in the Amazon—continue to face disproportionate infection rates, revealing persistent gaps in equity.
“Innovation must be equitable,” emphasized Dr. Carles Camon, Director of the Pan American Health Organization’s HIV unit. “Technology works only when it reaches every door, every neighborhood, every voice.” Europe and Central Asia report one of the most stable HIV curves, with new infections plateauing at roughly 170,000 annually—down significantly since the 1990s.
Western Europe benefits from universal health coverage, strong PrEP access, and national elimination strategies. Central Asian nations, however, are at a crossroads: despite declining rates, underreporting and limited service coverage in rural zones threaten long-term gains. The WHO forecasts risk of resurgence in these areas without targeted funding and policy reform.
Looking ahead beyond 2025, the WHO’s projections underscore a dual reality: with sustained funding, innovation, and political will, a future with fewer new infections and fewer deaths is biologically and socially achievable. Yet disparities in access to prevention, testing, and treatment maintain the risk of persistent pockets of epidemic activity, especially where human rights constraints limit freedom and healthcare reach. What does the 2025 projection truly reveal?
A pivotal window of opportunity to convert scientific advances into real-world impact—when marginalized populations gain full access, when political commitment matches epidemiological urgency, and when surveillance systems evolve to detect and respond faster than the virus spreads. As the global timeline draws near, HIV is no longer just a health crisis—it is a test of equity, resilience, and collective responsibility.
By 2025, global projections paint a landscape of fragile progress: new HIV infections may plateau near 1.3 million, but deaths will continue declining, signaling a critical shift in momentum.
Sub-Saharan Africa remains the epicenter, yet regional gains in treatment access and prevention show that transmission can indeed slow—if scaled sustainably. While inequalities persist, especially among marginalized groups in fragile regions, the data affirms that committed action, grounded in science and justice, can reshape the future of HIV. The problem is not insurmountable, but action is urgent and universal.

Related Post
Is Las Vegas in California? The Surprising Truth Behind Nevada’s Gambling Oasis

Unlocking Life’s Blueprint: What Is Biotic Potential?

Decoding Sonaria’s Creatures: The Life, Power, and Value of Creatures in the Creatures of Sonaria Value List
Corrina Jagger’s Life: A Legacy of Inspiration and Influence in <em>Bldur’s Greatest III</em> – The Unveiling of Evelyn’s Hidden Secrets

