Hisashi Ouchi’s Ordeal: When Nuclear Pain Became Medical Ethics’ Crucible
Hisashi Ouchi’s Ordeal: When Nuclear Pain Became Medical Ethics’ Crucible
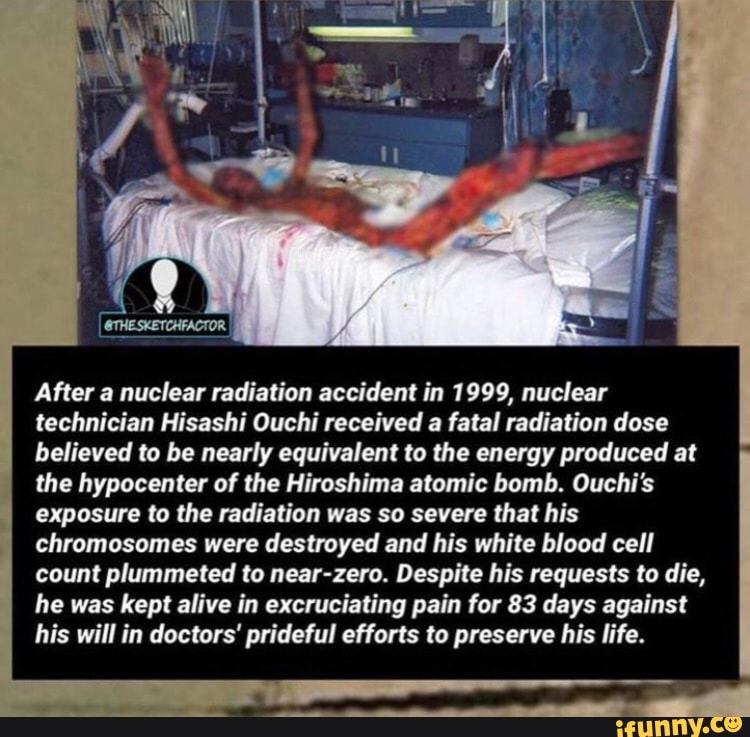
On September 29, 1999, a quiet cancer research facility in Tokai-mura, Japan, became the site of one of the most harrowing chapters in nuclear energy history—an accident that immobilized three workers in radioactive meltdown and ignited a profound reckoning with medical ethics, industrial responsibility, and human limits. Hisashi Ouchi, a 43-year-old technician, endured nearly eight weeks of excruciating exposure before succumbing to radiation sickness, embodying the visceral cost of technological failure and the moral weight borne by those who attempt to heal such wounds. His story—brutal, deeply human, and ethically charged—exposes the fragile intersection of science, suffering, and accountability in nuclear medicine.
When the sodium-cooled Fast Breeder Reactor (FBR) experienced a catastrophic coolant failure, radioactive sodium fused with zirconium cladding, triggering a massive fire that unleashed lethal radiation doses exceeding 17 sieverts—far beyond lethal thresholds. Ouchi, caught in the worst of the contamination, received mixed exposure across his skin, internal organs, and bloodstream, initiating a medical crisis exceeding all practical treatment limits. Over the following weeks, his body became a living laboratory, a testament to the brutal reality where radiology meets emergency medicine.
Medical professionals faced a dual dilemma: save Ouchi’s life while confronting the limits of medical science in combating extreme radiation injury. Standard protocols failed under the intensity of his exposure. Captured in Radiation Emergency Medical Management, the Tokyo Medical Center team operated in a space where every intervention carried life-or-death risk.
“We were treating symptoms without a path forward—radiation sickness at such levels had no proven cure,” recalled Dr. Naoto Okuda, lead physician involved in the case. “His symptoms included severe burns, bone marrow suppression, organ failure—but no treatment reversed the cellular decay unfolding inside him.”
The treatment regimen evolved from experimental to desperate.Early attempts at decontamination proved ineffective. Blood transfusions, stem cell support, and hyperbaric oxygen therapy were applied with limited success. Ouchi’s skin sloughed in layers as radiation reduced cellular integrity; his digestive tract failed, requiring continuous IV feedings laced with radiation-damaged cells.
Medical records show daily monitoring of critical metrics—white blood cell counts, hepatic function, and radiation absorption rates—each a grim barometer of survival probability. “We ran every protocol,” Okuda admitted. “But the biology of acute radiation syndrome at this scale defied containment.”
The ethical dimensions deepened rapidly.
With Ouchi slipping into irreversible multi-organ collapse, hospital ethics committees convened to debate continuation of care. Medical principles—beneficence, non-maleficence, and autonomy—clashed under extreme pressure. Family members, initially united in support, grappled with diverging views.
The reactor operator group and medical staff were divided: some argued prolonged treatment extended life at unbearable cost; others emphasized dignity and quality of stopover. “No one anticipated this,” said Ouchi’s colleague, a radiation safety officer. “We aimed to honor commitment, not ignore reality—but reality was cruel.”
Ouchi’s final days illuminated the visceral anxiety radiating through medical crisis management.His body betrayed increasing frailty: hair loss, dehydration, and fractures from minimal trauma. Medical imaging revealed genome-level damage—chromosomal breaks visible within hours of exposure, confirmed by specialized cytogenetic analysis. “He was not just a victim—he was a living timeline of radiation’s destruction,” noted Dr.
Kenji Matsuda, a molecular biologist reviewing the case ex post. “His cells told a story of acute damage no textbook fully described.”
Hisashi Ouchi died on November 21, 1999—just 262 days after initial exposure—his death marking both a personal and institutional failure in nuclear safety and emergency response. The aftermath spurred sweeping reforms in Japan’s nuclear regulatory framework, mandating enhanced safety systems, independent oversight, and stricter protocols for radiation incidents.
But beyond policy, Ouchi’s case redefined medical ethics in extreme radiation emergencies. It underscored that while science advances, certain limits remain immutable—where technology fails, science and conscience must confront the unspeakable with humility.\n\n
Scientific Mechanisms of Radiation Injury: A Tale of Cells Under Siege
The destruction in Ouchi’s body stemmed from acute ionizing radiation overwhelming cellular repair mechanisms. At extreme doses, high-energy neutrons and gamma rays devastated DNA, creating double-strand breaks too complex to repair efficiently.Within hours, hematopoietic stem cells in bone marrow—critical for blood cell production—collapsed, triggering pancytopenia and increased infection risk. Internal organ systems, particularly the gastrointestinal lining, suffered rapid epithelial necrosis, impairing nutrient absorption and immune defense. Organ failure ensued not merely from direct cell death but from cascading biochemical chaos: oxidative stress, inflammation, and apoptosis imitating continuous cellular self-deportation.
Current radiation medicine identifies no definitive threshold for irreversible damage at such scales—Ouchi’s case exceeded 10–20 sieverts, where survival chances plummet sharply. While experimental treatments like cytokine therapy and experimental hematopoietic stem cell grafts offered partial relief, none reversed the systemic devastation at play. The body, built for homeostasis, could not sustain the onslaught, transforming medical care into an ongoing battle against molecular collapse.
Ethics in Extremis: The Moral Weight of Deciding Who Lives
Medical teams confronted a profound ethical quagmire when treatment offered no clinical hope yet remained legally and morally incumbent upon them. Traditionally, life-saving care applies only when benefit exceeds risk; Ouchi’s case inverted this: survival offered no meaningful benefit, only prolonged suffering without cure. Each transfusion, every IV, extended fragile tissue survival but fueled a cycle of medical intervention without therapeutic closure.The principle of non-maleficence—“do no harm”—clashed with beneficence, demanding actions that prolonged existence yet inflicted pain. Legal frameworks in Japan reinforced this tension: no explicit mandate required life support withdrawal in ambiguous end-of-life scenarios. Ethics committees, composed of radiation experts and bioethicists, agonized over whether continuing care perpetuated futility or honored human dignity.
Family members, torn between hope and loss, weighed options amid emotional duress. The absence of a universal radiation triage protocol magnified uncertainty, exposing the fragility of consensus in extreme emergencies. This crisis revealed radiation medicine’s uncharted ethical frontier: where science limits healing, moral courage must guide decisions beyond survival calculus.
Legacy and Lessons: Rebuilding Safety and Ethics in Nuclear Medicine
The Tokai-mura disaster reshaped Japan’s nuclear safety apparatus, dismantling complacency through institutional reforms. The Nuclear Safety Commission imposed stricter contingency planning, independent auditing, and emergency medical response drills integrated into reactor operations. Public trust eroded—prompting broader societal debate over nuclear energy’s role—but transparency and accountability became cornerstones of renewal.Ethically, Ouchi’s ordeal elevated medical responsibility in radiological emergencies. Protocols now emphasize pre-established criteria for treatment limitation, guided by interdisciplinary ethics panels trained to act swiftly when esperance of cure vanishes. Research intensified on radiation countermeasures—targeted radioprotectants, advanced stem cell mobilization, and real-time genomic monitoring—seeking to bridge the gap between damage and repair.
Though no intervention can fully reverse severe radiation injury, collective memory ensures scientific rigor and moral reflection remain inseparable in high-stakes environments. Hisashi Ouchi’s sacrifice, in its agony and silence, affirms that progress demands not only technological mastery but unwavering compassion and clarity in crisis.}



Related Post

Isaiah 61: The Prophetic Promise of Healing, Restoration, and Divine Replenishment
Jeff Foxworthy’s Net Worth: From “You Might Be from Alabama” to billion-dollar country music stardom

Tamara Romijn: A Comprehensive Insight Into the Life and Career of a Trailblazing Force

Lamar Jackson Collegiates: The Dynamic Force Behind Israeli Basketball’s Rising Stars