HIV-2 Positive: What Your Test Results Truly Mean
HIV-2 Positive: What Your Test Results Truly Mean
Sentensions run high when a diagnostic test returns an HIV-2 positive result—an outcome that carries distinct biological, clinical, and personal implications. Unlike the more widely recognized HIV-1, HIV-2 is less common but no less significant, requiring nuanced understanding to navigate testing, prevention, and long-term health management. Understanding your HIV-2 positive status is not just about accepting a label—it’s about gaining critical insight into your immune health, transmission risks, and treatment pathways.
Coming to terms with these results demands accurate knowledge, clear context, and compassionate support.
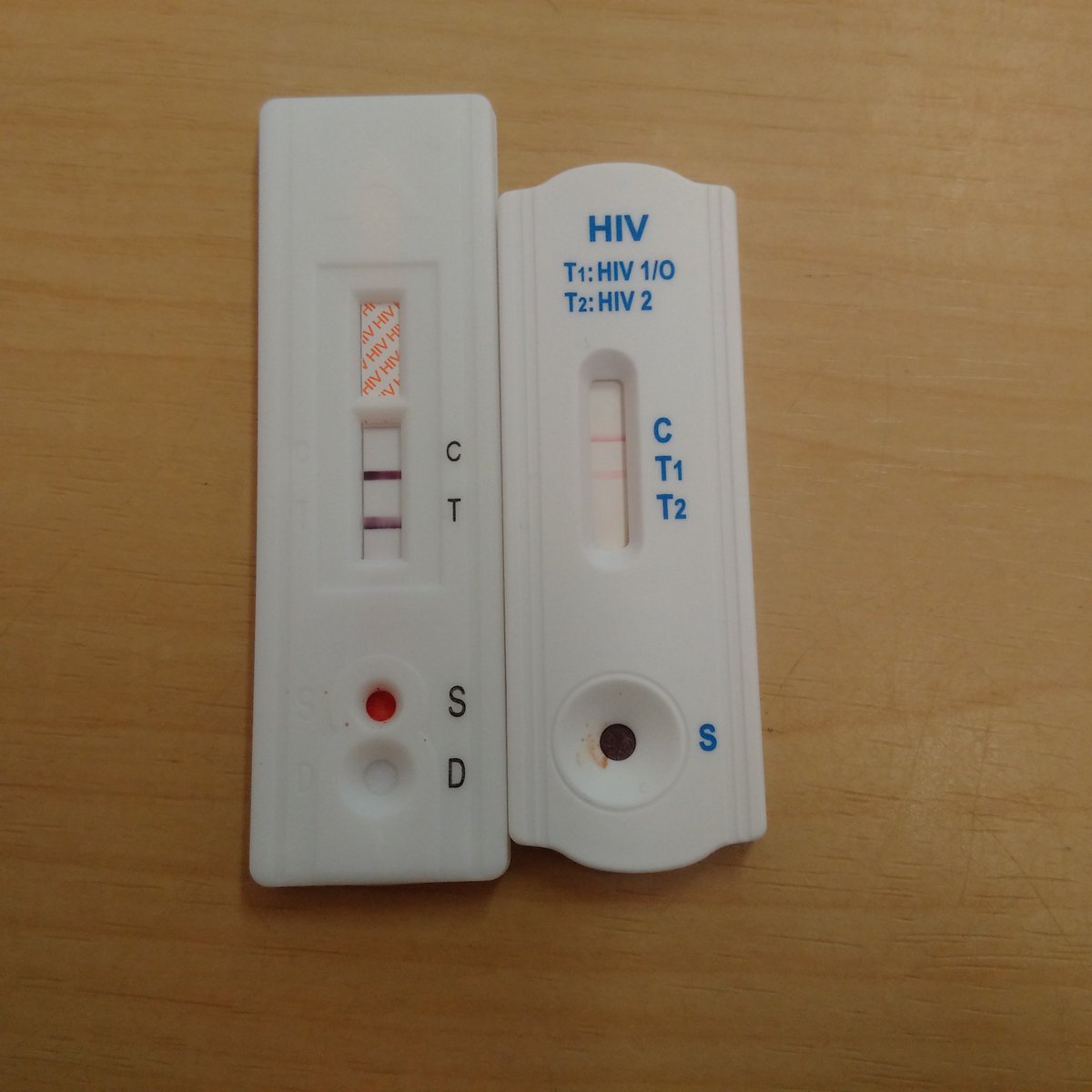
Decoding the HIV-2 Positive Result: Key Test Components
An HIV-2 positive result from standard screening reflects positivity to HIV-2 antibodies, typically detected by enzyme immunoassays (EIAs). However, confirmation requires follow-up testing—usually a HIV-2 specific Western blot or a nucleic acid test (NAT)—to distinguish true infection from false positives and to characterize viral load.“HIV-2 antibodies develop more slowly than HIV-1 in many individuals,” explains Dr. Maria Thompson, an infectious disease specialist. “This delayed seroconversion means early tests may miss infection, especially if drawn too soon after exposure.” Testing methodologies vary, and understanding which assays were used can clarify result reliability.
Results are often reported in reference ranges: a positive HIV-2 test is confirmed if viral markers fall within a defined cutoff—typically a bound HIV-2-specific antigen-antibody complex, or a qualitative band on blot analysis. The test’s specificity and sensitivity influence accuracy, with modern platforms generally exceeding 99% in confirming active infection. Yet, a “positive” alone does not reveal the full clinical picture—neutralizing antibodies, viral load, and CD4 counts provide essential layers of insight.
HIV-2 vs. HIV-1: Biological and Epidemiological Differences
HIV-2 and HIV-1 differ significantly in origin, transmission dynamics, and global distribution. HIV-2 emerged from cross-species transmission of SIV from sooty mangabeys in West Africa, spreading primarily in Guinea-Bissau, Senegal, and parts of Brazil.In contrast, HIV-1 originated from multiple SIV strains in central Africa and became a worldwide pandemic. “HIV-2 is generally less transmissible and progresses more slowly than HIV-1,” notes epidemiologist Dr. Kwame Osei.
While HIV-1 drives most global cases, HIV-2’s distinct biology influences clinical monitoring. Clinically, HIV-2 infections often present with milder early symptoms and slower disease progression, though this varies widely among individuals. The virus replicates more slowly, meaning time-to-diagnosis (ΔNT) for HIV-2 can be months longer than for HIV-1.
This affects screening protocols: standard HIV-1 tests often miss early HIV-2 infections unless specifically designed. “Many sexual health clinics now offer dual HIV-1/HIV-2 testing to prevent missed diagnoses,” Osei adds. These differences underscore why an HIV-2 positive result demands specialized clinical interpretation beyond standard HIV-1 guidance.
What Your Test Results Really Reveal
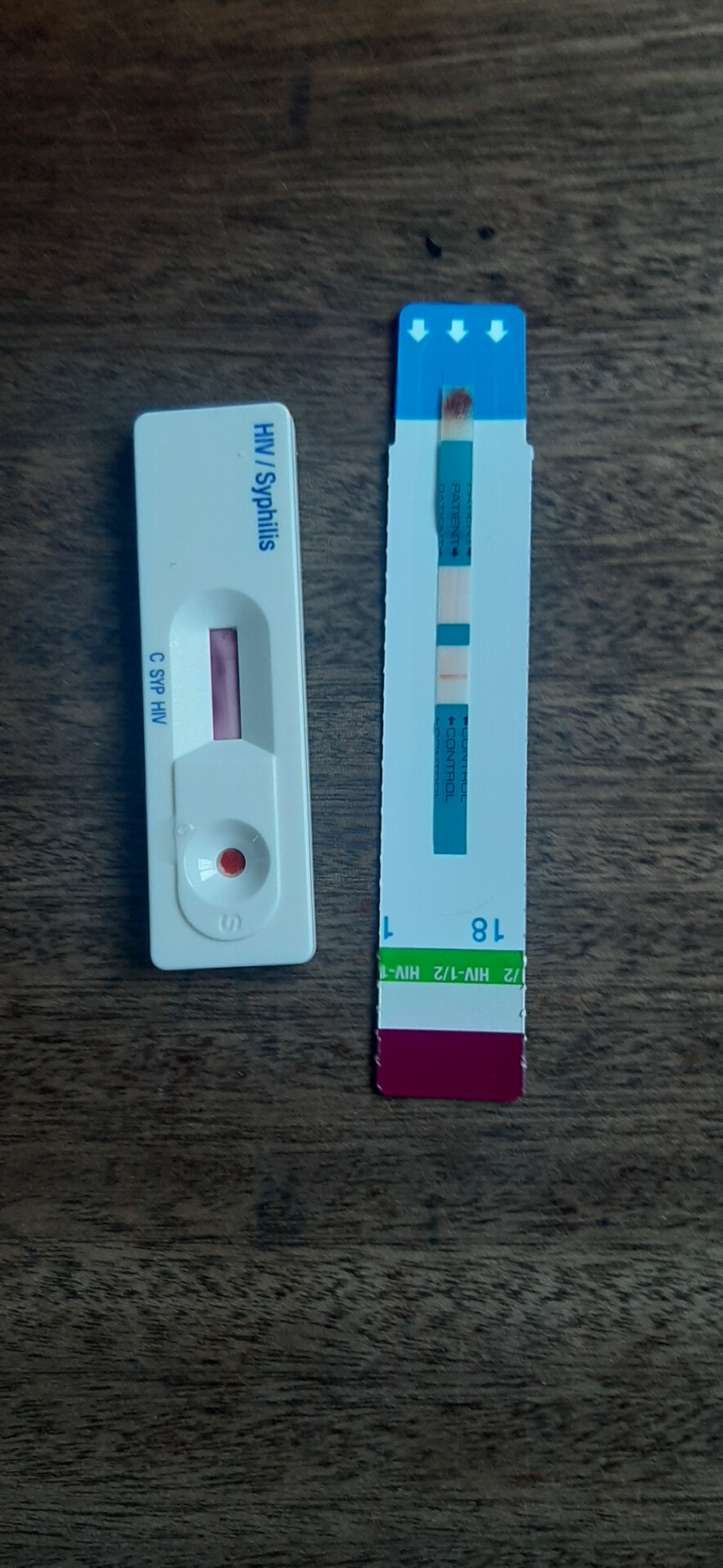
A positive HIV-2 result signals exposure to the virus, but understanding its progression and impact hinges on a full laboratory profile. Key data points include: - **Viral Load (HIV-2 RNA)**: Measures active viral replication; higher levels correlate with increased transmission risk and faster immune decline in untreated cases. - **CD4 T-Cell Count**: Indicates immune system strength; declining counts mark advancing disease and inform treatment timing.- **Specific Antibody Subtypes**: Identifies whether the virus strain aligns with HIV-2 groups (A, B, or others), influencing regional epidemiology and potential drug resistance patterns. - **Co-infections and Comorbidities**: Testing often includes screening for Hepatitis B, Hepatitis C, syphilis, and tuberculosis, vital given overlapping transmission routes and immune effects. “Viewing a result in isolation risks misdiagnosis,” warns Dr.
Thompson. “For example, a low CD4 count paired with early HIV-2 RNA detectable on a responsive test may signal acute infection—requiring urgent intervention.” Timely, comprehensive testing enables early detection and personalized care plans.
Transmission, Risk, and Personal Health Management
Despite lower transmissibility compared to HIV-1, HIV-2 can spread through unprotected sex, blood exposure (e.g., shared needles), and maternal-fetal transmission.However, its lower viral load in blood and slower replication generally reduce transmission potential outside high-risk contexts. “People with HIV-2 can live long, healthy lives with early, consistent antiretroviral therapy (ART),” says Dr. Osei.
Viral suppression through treatment not only protects personal health but also eradicates sexual transmission risk “essentially eliminating the chance of passing the virus,” according to prevention guidelines. For those newly diagnosed, early education about the virus becomes critical. STD clinics and healthcare providers play a key role in explaining how HIV-2 differs从势 from HIV-1 in transmission prevention, symptoms, and long-term outlook.
Adherence to ART remains central: studies confirm that consistent treatment reduces viral load to undetectable levels within months, minimizing immune damage and complications.
Navigating the Emotional and Social Impact
Receiving an HIV-2 positive result often triggers complex emotional responses—fear, stigma, uncertainty. Yet, modern medicine and public health efforts emphasize that a positive diagnosis is not a life sentence.“Many individuals with HIV-2 live full, active lives with appropriate care,” notes Dr. Thompson. Support systems, including counseling, peer networks, and medical advocacy, are vital in reducing psychological burden and enhancing treatment adherence.
Socially, misconceptions about HIV-2 persist, sometimes fueled by its relative rarity. “People mistakenly believe HIV-2 is ‘milder’ than HIV-1 and thus less concerning—but this oversimplification can delay critical care,” cautions Dr. Osei.
Awareness campaigns stress that while HIV-2 may progress more slowly, each diagnosis demands vigilance, personalized treatment, and community support. Stigma remains a silent barrier; open, fact-based dialogue helps foster understanding and reduces isolation.
Ready for Action: Next Steps After a Positive HIV-2 Result
Following a confirmed HIV-2 positive test, the immediate focus is on clinical validation and care initiation.Core steps include: - Confirmatory testing to rule out false positives and characterize virus subtype. - Baseline laboratory assessment: CD4 count, viral load, full STD panel, and hepatic function tests. - Entry into a care network with an infectious disease specialist experienced in

Related Post
What Visible Signs Reveal a Precipitation Reaction: The Science Behind the Spark in Tests

Unleash Snow Rider 3D in Unblocked GitHub: The Wild Simulation You Never Knew You Needed

David Centner’s Net Worth: The Disciplined Blueprint Behind a Financial Empire
Unveiling Brittany Jade Szabo’s True Net Worth: The Untold Truth Behind Her Growing Empire

