Navigating the Fight Against African Sleeping Sickness: Current Treatment Options and Realistic Patient Expectations
Navigating the Fight Against African Sleeping Sickness: Current Treatment Options and Realistic Patient Expectations
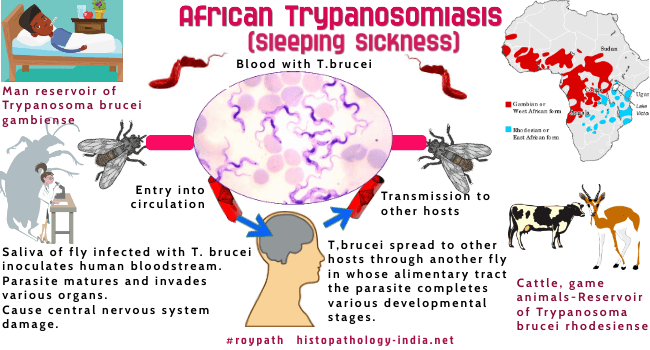
African trypanosomiasis, commonly known as sleeping sickness, is a relentless parasitic disease transmitted by the bite of tsetse flies across tropical regions of sub-Saharan Africa. Caused by species of the parasite *Trypanosoma*, the infection progresses through two distinct phases—haemolymphatic (early) and meningoencephalitic (late)—with severe neurological complications if untreated. The disease is not only a public health challenge but also a test of global health responses, where timely diagnosis and access to treatment remain critical.
Despite advances in medical science, patients and caregivers continue to face uncertainty about therapeutic options, recovery timelines, and long-term outcomes. This article explores the current treatment landscape and what individuals affected by sleeping sickness can realistically expect during diagnosis, therapy, and recovery.
Diagnosis typically begins with a thorough clinical evaluation, especially given the nonspecific early symptoms—fever, headaches, swollen lymph nodes, and fatigue—that often mimic common illnesses.
Blood samples undergo serological testing, including enzyme-linked immunosorbent assays (ELISA) and indirect immunofluorescence, to detect parasite-specific antibodies. In later stages, where trypanosomes appear in cerebrospinal fluid (CSF), a Lymphocyte Transformation Test (LTT) confirms CNS involvement. Early and accurate detection remains a cornerstone, yet diagnostic delays are still widespread due to limited healthcare infrastructure in endemic zones.
"Many patients do not seek care until symptoms escalate, by which point treatment options grow more complex and risks increase," notes Dr. Amina Diallo, a tropical disease specialist at the World Health Organization.
From Stage-Specific Therapies: The Arsenal Against Trypanosoma Parasites
The choice of treatment depends largely on the disease stage, parasite species (*T.brucei gambiense* or *T. brucei rhodesiense*), and patient-specific factors. The WHO’s recommended regimens reflect decades of clinical research and evolving pharmacological innovation.
The haemolymphatic phase—characterized by systemic spread without CNS invasion—responds to first-line drugs such as arsenicals, pentamidine and suramine. Among these, eflornithine-cetrimide (Efl الطبي) has emerged as a breakthrough: FDA-approved in 2016 for early-stage *T. b.
gambiense* infection, it delivers higher efficacy with fewer neurological side effects compared to older pentamidine. "Eflornithine represents a major step forward—it’s not just effective, it’s safer," said Dr. Diallo.
For late-stage *T. b. rhodesiense* or when haemolymphatic treatment fails, nifurtimox-ethyl (Nifurtimox-Ethionicamide) remains the cornerstone, though its use demands careful monitoring due to dose-limiting toxicities.
In the meningoencephalitic phase—where parasites breach the blood-brain barrier—treatment becomes more delicate. Cerebral involvement significantly complicates management, increasing the risk of fatal neurological complications even with optimal therapy. Arsenals like melarsoprol, historically the primary option, carry high rates of severe neurotoxicity, requiring slow infusion and close neurological surveillance.
Newer combinations pairing eflornithine with nifurtimox are being studied, but protocol standardization remains limited. “Armed with eflornithine for early CNS disease is transformative, yet for late-stage, it’s about balancing sharp parasite killing with managing debilitating side effects,” explains Dr. Kwame Nkosi, a medical entomologist involved in WHO treatment guidelines.
While traditional chemotherapy dominates the current paradigm, innovative research explores next-generation therapies and adjunctive strategies. Novel drugs in preclinical and clinical trials target parasite metabolism, replication, and immune evasion mechanisms. For example, compounds inhibiting glycosome function—essential energy-producing organelles in trypanosomes—show promising results in animal models.
Additionally, immunotherapeutic approaches, including monoclonal antibodies and vaccines, are under investigation to boost host defenses and prevent relapse. Although none have yet reached widespread use, these developments offer hope for simpler, more tolerable regimens of the future.
What Patients Can Expect: Timeline, Side Effects, and Recovery Realities
Managing sleeping sickness requires clear expectations across medical, physical, and emotional domains.The treatment timeline varies: early-stage patients typically begin therapy within days and achieve symptom improvement within 2–4 weeks, with complete parasite clearance detectable via CSF testing. Late-stage cases demand prolonged treatment—often 6 months or more—requiring sustained outpatient monitoring to track response and toxicity.
Medication side effects are a prominent concern.
Arsenicals like eflornithine may cause skin rash, taste disturbances, and transient fatigue, while nifurtimox introduces gastrointestinal upset, nausea, and in rare cases, severe hepatotoxicity. Melarsoprol, though less used today, remains notorious for peripheral neuropathy and encephalopathy. “Each patient’s tolerance varies,” notes Dr.
Diallo, “so clinicians tailor dosing, use supportive care, and pause treatments if complications arise.” Recovery extends beyond clinical markers. Neurological sequelae—such as cognitive impairment, memory deficits, and motor coordination issues—affect up to 30% of survivors, even after successful therapy. Post-treatment support often includes neuropsychological rehabilitation, physical therapy, and community reintegration programs.
Psychosocial stressors, stigma, and economic hardship compound these challenges, underscored by narratives like that of a Ugandan farmer who, after years of fatigue and confusion, found renewed purpose through structured health and work support.
Long-term follow-up remains essential. Serological reactivation may occur, requiring surveillance, especially in endemic areas.
Patients benefit from awareness campaigns that educate communities on early symptom recognition and prompt care-seeking, reducing irreversible progression.
The Path Ahead: Bridging Gaps in Access and Innovation
Despite robust treatment frameworks, substantial barriers persist. Geographical remoteness, health system fragility, and limited trained personnel delay diagnosis and treatment initiation.WHO data indicate that only about 30% of at-risk populations receive timely care, with regional disparities marked by lower access in Congo Basin and Sahel regions. Investment in point-of-care diagnostics, decentralized treatment models, and community health worker training holds transformative potential. Integration with broader primary care enhances screening efficiency.
Concurrently, global collaboration drives drug development: partnerships between African research centers and international pharmaceutical entities accelerate clinical trials and regulatory approval. Looking forward, the goal is not merely treatment, but prevention and elimination. Vaccination research, vector control innovations—such as sterile insect techniques—and surveillance enhancements together form a comprehensive strategy to reduce transmission and eventually eradicate sleeping sickness.
In sum, AFrican trypanosomiasis remains a complex but treatable condition with evolving therapeutic paradigms. Patients can expect targeted, stage-appropriate interventions that, while demanding, offer real hope for recovery when caught early and supported holistically. Advances in medicine, combined with strengthened health systems and inclusive policies, are reshaping the trajectory of this historical disease—turning once-fatal diagnoses into manageable health challenges.
With continued investment and global commitment, sleeping sickness is not only conquerable but preventable.



Related Post

Twitches: Where Skill, Community, and Magic Converge in the Live-Streaming Revolution

Emily Ratajkowski’s Power and the “Blurred Lines”: When Art, Controversy, and Cultural Shock Collide

Eben Byers Drank Radioactive Water and Didn’t Regret a Single Sip—Until He Said “45 OFF

Mickey Guyton American Idol Bio Wiki Age Husband

