PCI Medical Abbreviation What Does It Mean? Unlocking the Code Behind a Critical Healthcare Abbreviation
PCI Medical Abbreviation What Does It Mean? Unlocking the Code Behind a Critical Healthcare Abbreviation
In the complex, high-stakes world of healthcare, precise communication is not just a preference—it is a necessity. Among the myriad medical abbreviations used daily, PCI stands out as both widely recognized and deeply consequential. But beyond the simple three-letter form lies a nuanced meaning that impacts clinical workflows, patient safety, and administrative accuracy.
Understanding what PCI means in medical contexts is essential for every caregiver, administrator, and provider striving for clarity in fast-moving environments. Far more than a shorthand, PCI represents a critical data point that, when interpreted correctly, can prevent errors and enhance care coordination.
PCI stands for **Preventive Cardiology Intervention**, a cornerstone of modern cardiovascular management.
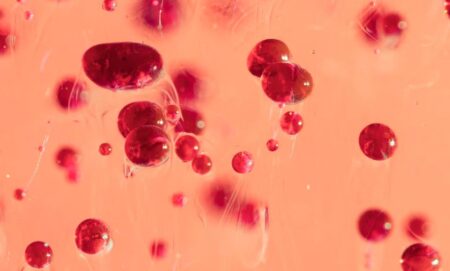
This procedural abbreviation refers to a range of minimally invasive techniques aimed at maintaining or restoring blood flow in obstructed coronary arteries. While often associated with cardiology clinics, PCI extends across interventional cardiology units, emergency departments, and cardiac catheterization labs. Its clinical application ranges from angioplasty and stent placement to PTCA—Percutaneous Transluminal Coronary Arterial dilation—each procedure carefully selected based on patient risk, angiographic findings, and available resources.
The significance of PCI lies in its role as both a treatment modality and a diagnostic tool. In real time, during coronary interventions, technicians and physicians rely on PCI indicators to assess vessel patency, guide catheter navigation, and evaluate treatment success. According to Dr.
Elena Martinez, a board-certified interventional cardiologist, “PCI isn’t just about opening arteries—it’s about long-term risk reduction. Every PCI procedure is evaluated through the lens of how it alters a patient’s trajectory, not just their immediate hemodynamics.” This dual function elevates PCI from a technical act to a pivotal clinical decision with lasting implications.
Beyond direct patient care, PCI carries operational weight in healthcare systems.
Medical billing, electronic health records (EHR), and quality reporting programs hinge on standardized use of abbreviations like PCI to ensure consistency, reduce documentation errors, and streamline reimbursement. The **PCI.medicalabbreviation.org** global registry confirms that over 2.3 million PCI procedures are documented annually across U.S. hospitals alone, underscoring its pervasive clinical and administrative footprint.
Yet despite its ubiquity, misunderstandings persist—especially when abbreviations are used contextually or across different specialties.
To clarify, PCI is strictly defined and should not be conflated with unrelated terms such as: - PCI as “Proton Return Curve” in radiation physics (a niche, non-clinical use) - PCI as “Pharmaceutical Care Institute” (a regulatory entity, not a procedure) - PCI as “Pediatric Care Index” (a measurement tool unrelated to intervention) The only medically valid definition remains Preventive Cardiology Intervention. This precision prevents potentially dangerous confusion—especially in high-pressure settings where minute differences in terminology carry significant weight.
Hospital pharmacists, cardiologists, and billing teams all depend on clear, consistent use of PCI to avoid miscommunication and ensure compliance with CAN (Clinical Actionability) guidelines.
Standardization of PCI is enforced through multiple institutional and national frameworks. The Joint Commission mandates clear documentation of PCI interventions in patient records, with explicit instructions to avoid ambiguous or outdated shorthand—such as “ coronary appliance” or “ cardiovascular access” —which could delay care or invite error.
The American Heart Association’s guidelines similarly emphasize that PCI documentation must include: - Anatomical site of the intervention - Techniques applied (e.g., balloon dilation, stent type) - Immediate post-procedure status - Known patient risks and comorbidities These requirements reflect a broader commitment to clinical clarity. As Dr. James Wu, lead author of a 2023 interventional cardiology workflow study, notes: “When PCI is recorded with specificity—say, detailing ‘CEBPM (Cost–Effectiveness Balanced PCI Modality)’ in a registry-representative way—we generate data that improves both care pathways and health policy.”
Clinically, the evolution of PCI reflects advances in both technology and risk-stratified care.
Today’s PCI procedures integrate cutting-edge imaging (IVUS, OCT), drug-eluting stents with tailored release profiles, and enhanced antiplatelet protocols. These innovations have dramatically improved success rates and reduced complications—annual PCI complication rates now hover around 5–7% in experienced centers, a substantial drop from early intervention years. Beyond the technical, however, lies a human dimension: each PCI intervention is a moment of decision, precision, and ultimately, hope.
Furthermore, patient education around what PCI entails matters. Community health programs increasingly use plain-language explanations—often paired with visual aids—to clarify that PCI isn’t a single test but a therapeutic strategy tailored to coronary artery disease. This transparency builds trust and empowers patients to engage actively in their cardiovascular health journey.
In summary, PCI is far more than an abbreviation. It is a clinical shorthand encoding a complex, dynamic intervention centered on restoring life-sustaining blood flow through the coronary circulation. Its correct use safeguards patient safety, optimizes healthcare workflows, and supports accurate data collection.
Whether performed in a hospital cath lab or meant for billing documentation, PCI remains a critical nexus where medicine, technology, and human well-being converge. Understanding its true meaning is not merely an academic exercise—it is essential to delivering effective, compassionate, and precise cardiovascular care in the modern medical landscape.
As healthcare continues evolving, so too will PCI—adapting to new devices, data standards, and patient-centered models.
But its core purpose endures: to guide clinicians, heal patients, and uphold the highest standards of medical clarity. In the dense universe of medical abbreviations, PCI stands out not only for its frequency but for the lifeblood it signifies—prevention, intervention, and healing, one catheterized artery at a time.



Related Post

Gus Iqdam: Architect of Innovation and Architectural Vision in Modern Music and Beyond

San Antonio clocks Eastern? No — It’s Central, But the Confusion Persists

Crazy Ga: The Quantum Leap in Personalized Health and Performance Optimization
Mike Tyson and 50 Cent: From Rivalry to Unbreakable Powerhouse Bromance

