Stroke Don’t Miss the Moment By — When Every Second Counts
Stroke Don’t Miss the Moment By — When Every Second Counts
In the split second following a stroke, lives are transformed—before medical hands reach or the patient regains awareness. Sheryl Brady’s powerful message, “Don’t miss the moment by,” encapsulates a critical truth: timely recognition of stroke symptoms can save brain cells, preserve function, and alter recovery trajectories. Stroke remains one of the leading causes of long-term disability and death globally, yet public understanding of early warning signs often lags behind medical progress.
The rare but vital moment between onset and intervention demands immediate action—a moment Sheryl Brady insists we don’t afford to misjudge or waste. Time is a neurologist’s most precious currency. When a stroke strikes, brain cells begin to die within minutes due to interrupted blood flow.
Research shows that every 30 seconds without treatment reduces the potential for full recovery. Yet, far too many people delay help, misinterpret symptoms, or mistake them for less urgent conditions. “People often dismiss subtle signs—facial drooping, arm weakness, speech slurring—as tiredness or minor ailments,” explains Dr.
Maria Chen, a vascular neurologist at Johns Hopkins Medicine. “But those seconds matter. Acting fast isn’t just important—it’s survival.” The Save a Life Moment hinges on recognition and response.
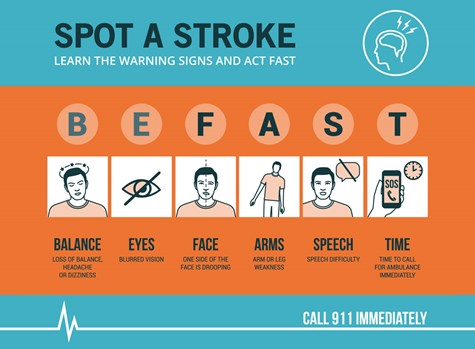
Sheryl Brady’s compelling call to “don’t miss the moment by” underscores a simple but profound idea: awareness must guide action. The American Stroke Association identifies the iconic F.A.S.T. mnemonic—Face, Arms, Speech, Time—as a global benchmark for identifying stroke symptoms quickly.
But beyond memorization, true readiness means internalizing the urgency. Many hesitate to call emergency services at the first red flag, fearing hospital costs, confusion over diagnosis, or embarrassment. Yet delaying intervention increases the risk of permanent disability or death.
“A ‘lucky’ outcome often starts not in the hospital, but in the home,” Brady emphasizes. “When someone notices a sudden numbness, slurred speech, or eye droop, they must act immediately—don’t wait for perfection in knowing.” Accessibility and education remain key challenges. Despite widespread knowledge of F.A.S.T., recent national surveys reveal persistence in delayed help-seeking behaviors.
Factors include confusion about stroke vs. other symptoms, cultural stigma around seeking emergency care, and geographic or socioeconomic barriers to rapid medical access. Brady’s message targets these gaps with urgency: “We can’t wait for perfect knowledge—we need widespread, actionable instinct.” Practical steps are clear.
The moment begins the second concerning symptoms appear—whether facial droop lasting seconds, sudden weakness in one limb, or incoherent speech. The response: call emergency services immediately and note the time of symptom onset. “Knowing when the last normal moment was helps providers act decisively,” says Emily Rodriguez, a public health educator focused on stroke prevention.
“There’s no room for doubt. This isn’t a ‘later’ moment—it’s now.” Technology and community play growing roles. Mobile apps, automated symptom checkers, and public awareness campaigns led by figures like Brady help bridge awareness and action.
Social media campaigns, particularly in underserved communities, have shown measurable success in reducing response delays. “When people hear from trusted sources—and see their neighbor or family member survive due to quick action—they begin to treat stroke as a life-or-death priority,” says Dr. Chen.
Real stories reinforce this call. Take the case of Maria Gonzalez, a 67-year-old teacher in Miami, who recognized stroke signs in her 59-year-old brother within minutes. “He had slurred speech and could lose movement in his right arm,” she recalls.
“Instead of questioning myself, I grabbed my phone and dialed 911 the second symptoms started. They arrived in under 15 minutes. Today, he’s recovering because of that choice.” Such experiences illuminate what Brady warns against losing: precious moments slipping by through hesitation or misunderstanding.
Healthcare systems are adapting to shorten response windows. Stroke centers equipped with rapid imaging and clot-busting therapies now operate within 90-minute benchmarks. Yet these advances mean little without community vigilance.
Brady’s message targets both individuals and institutions: every person must become a potential first responder, every community a frontline network of awareness. The moment matters not only in terms of minutes past symptom onset but in cultivating a culture of preparedness. From school classrooms to workplace training, education on stroke recognition and emergency action is saving lives.
“It’s not about perfection,” Brady states plainly. “It’s about presence—being ready to act when it counts.” In an age of instant information, the critical challenge remains translating awareness into instant action. Don’t miss the moment by waiting, second-guessing, or doubting.
Don’t miss it by ignoring subtle cues or delaying care—because in stroke, the gap between symptom and treatment can define life or death. Sheryl Brady’s powerful refrain is unmistakable: act now, act fast, act with purpose. The window may be narrow, but it is always open—for those who know and act.
Whether recognizing facial weakness, sudden confusion, or arm drift, don’t wait. “Don’t miss the moment by,” your voice must echo—for you, for your loved ones, for every second that shapes recovery. In stroke, time waits for no one—only readiness answers.


Related Post

Shanda Vander Arks Son’s Life Through the Lens — A Visionary Journey Captured by Rk’s Powerful Gallery
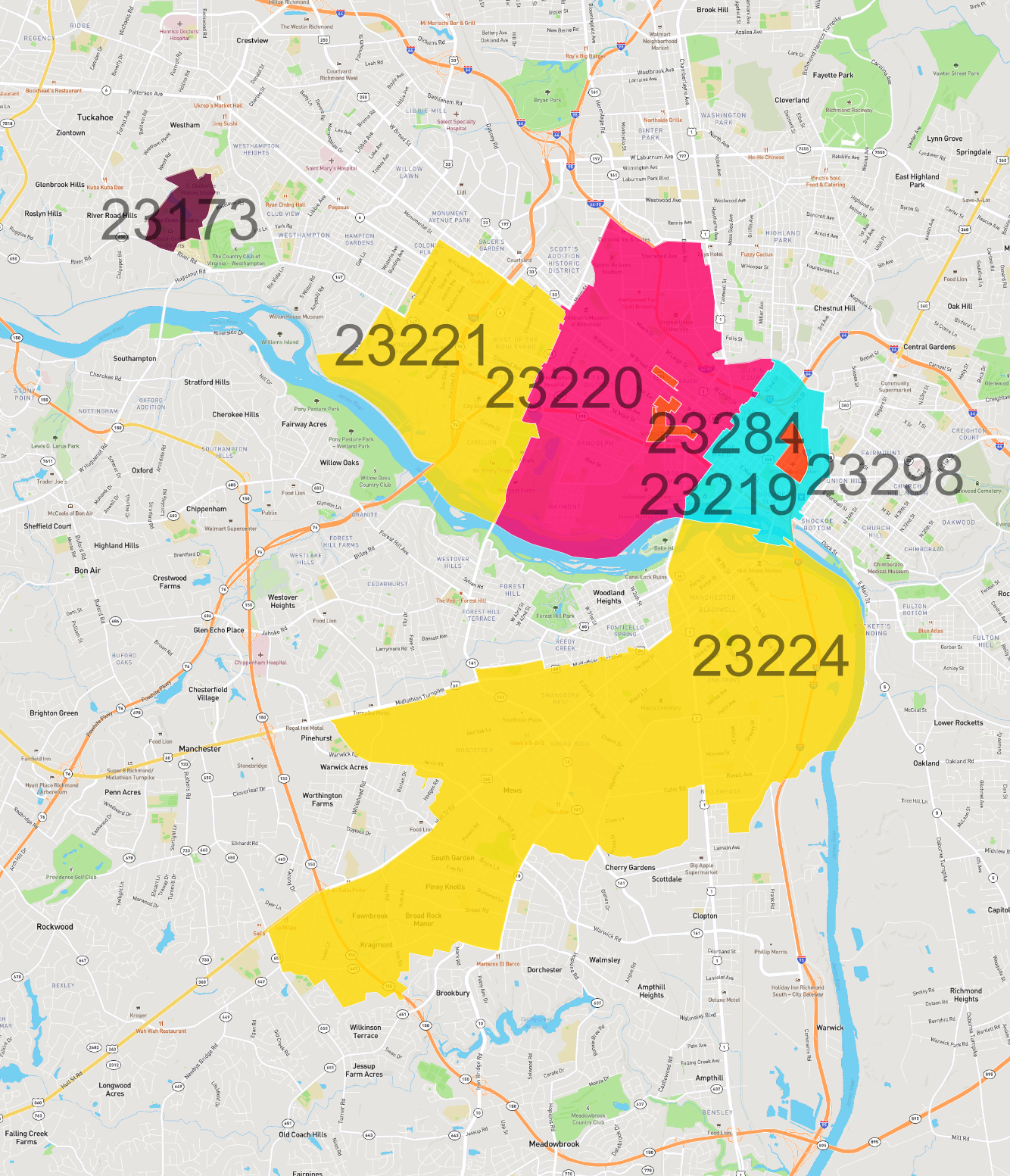
Richmond VA Zip Codes A Quick Guide: Master Your Neighborhood Code
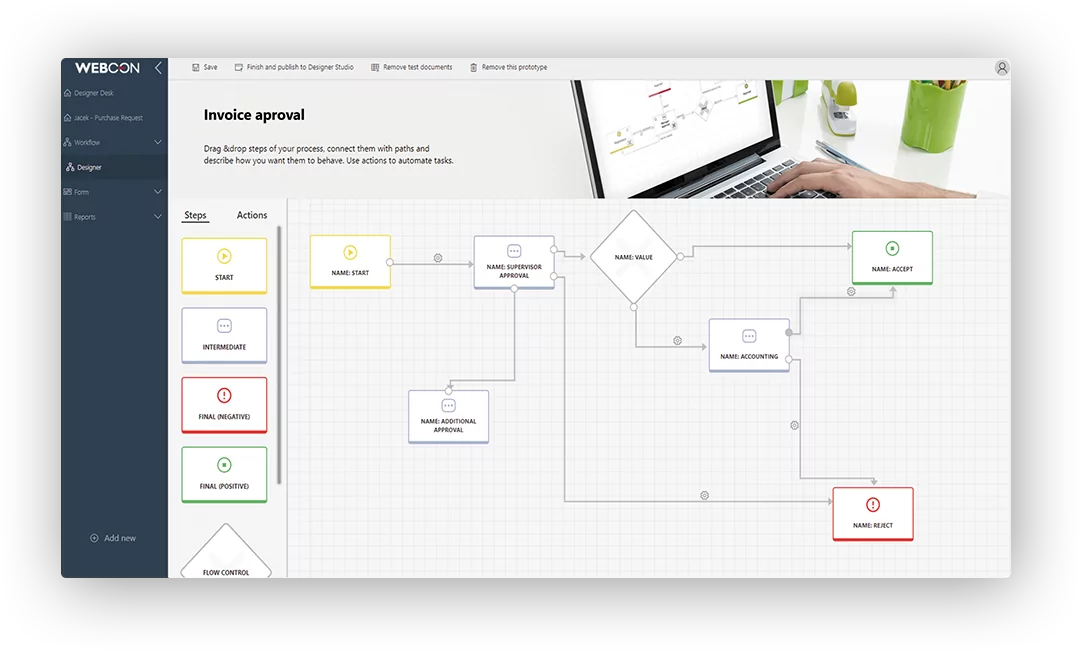
Smart Switch on Application Smart Switch: Revolutionizing Enterprise Workflow with Precision and Control

Quantum Computing Breaks Barriers: Current Milestones Propel Reality of Scalable Machines Forward

