Understanding Fluid Buildup In The Knee: Causes, Symptoms, And Treatment Options
Understanding Fluid Buildup In The Knee: Causes, Symptoms, And Treatment Options
When fluid accumulates inside the knee joint, it’s not just a minor discomfort—it’s a signal from the body that something is amiss. Often mistaken for simple swelling, fluid buildup in the knee, medically known as joint effusion, reflects underlying mechanical, inflammatory, or structural issues that demand attention. This article unpacks the complex interplay of factors behind this common yet frequently misunderstood condition, identifies key symptoms to watch for, and outlines the evolving range of treatment options, empowering individuals to act decisively on knee health.
What Is Fluid Buildup In The Knee and Why Should You Care?
Fluid buildup in the knee refers to excess synovial fluid accumulating within the joint space, a sanctuary normally filled with a precise amount to cushion movement, reduce friction, and nourish cartilage. While small amounts are normal, excessive fluid—when noticeable or recurrent—can restrict motion, trigger pain, and indicate damage beyond superficial irritation. The knee, a hinge joint under constant stress during walking, running, and bending, is particularly vulnerable to imbalances that tip fluid dynamics.Understanding both the biological mechanism and the clinical implications is essential for timely intervention. The synovial cavity, where fluid resides, relies on a delicate balance. Under normal conditions, synovial membrane secretes fluid in response to movement and load, maintaining lubrication.
When inflammation, injury, or degenerative changes disrupt this equilibrium, fluid production surges while absorption lags—resulting in pressure buildup. Clinically, this manifests not only as visible swelling but also as stiffness, warmth, and reduced range of motion.
Common Causes Behind Knee Fluid Accumulation
Fluid buildup arises from diverse origins, ranging from acute trauma to chronic degenerative processes.Identifying the root cause is critical for directing treatment. Key triggers include: - **Injury-Related Effusion** Lie medical events such as ligament tears (e.g., ACL rip), meniscal injuries, or dislocations are frequent initiators. Trauma inflames synovial layers, prompting increased fluid secretion.
For instance, a rupture in the medial collateral ligament often triggers rapid swelling within hours, as blood vessels leak into the joint space. - **Osteoarthritis (OA)** The most prevalent cause among older populations, OA damages cartilage, letting bony surfaces grind. This mechanical wear irritates synovial tissue, prompting persistent fluid production.
“In OA, the joint is effectively “blind” to fluid regulation—each movement amplifies irritation,” notes Dr. Elena Torres, a sports medicine specialist. - **Rheumatoid Arthritis (RA)** An autoimmune disorder, RA inflames synovial membranes globally, causing thickened, fluid-filled tissue.
The effusion here is not just serum but an inflammatory exudate rich in immune cells, contributing to joint distortion over time. - **Infection (Septic Arthritis)** A medical emergency, infected joints flood with white blood cells, pus, and fluid, often accompanied by heat, redness, and sharp pain. Prompt diagnosis is vital to prevent irreversible joint destruction.
- **Post-Surgical or Inflammatory Response** Following procedures like ligament repair or total knee replacement, fluid may accumulate as part of healing—or signal complications like infection or capsule tightness. - **Gout and Crystal Deposition** Uric acid crystals settle in joints, triggering inflammation and fluid buildup. This classic “tophi” formation, often in the knee’s posterior surface, presents with sudden swelling and intense pain.
Understanding these origins allows clinicians to tailor diagnostics and interventions, moving beyond symptom management to root-cause correction.
Recognizing The Symptoms: When To Seek Medical Attention
Symptoms of fluid buildup vary by cause but commonly include: - **Visible swelling** — Visiblelut diminished skin tightness, especially around the joint line. - **Stiffness and tightness** — The knee may feel “stuck” or resistant to bending, particularly after rest.- **Pain** — Ranging from dull aches to sharp discomfort, often worsened by movement or pressure. - **Limited range of motion** — Difficulty fully straightening or flexing the knee, reducing functional capacity. - **Warmth or redness** — Indicative of inflammation or infection, requiring urgent evaluation.
- **Popping or catching sensations** — Suggests mechanical compromise from torn cartilage or loose bodies. Chronic cases may reveal subtle clues: morning swelling that eases by midday signals inflammatory arthropathies, while persistent fluid without injury warrants screening for tumors or metabolic disorders. Early symptom awareness dramatically improves outcomes.
Diagnosis and Diagnostic Tools for Fluid Accumulation
Pinpointing the cause of knee effusion demands a multi-faceted diagnostic approach: - **Physical Examination** — Palpation identifies tenderness, warmth, and joint line tenderness. Passive range-of-motion tests assess functional limitations. - **Imaging Studies** — X-rays detect joint space narrowing or bony changes indicative of OA or trauma.MRI provides detailed views of soft tissues, revealing meniscal tears or synovial thickening unseen on X-ray. Ultrasound enables real-time fluid visualization and guides needle placement for drainage. - **Arthrocentesis — Fluid Analysis** — Aspirating synovial fluid clarifies etiology: clear fluid suggests OA, cloudy or bloody fluid points to infection or hemarthrosis, while uric acid levels confirm gout.
- **Blood Tests** — Elevated inflammatory markers (CRP, ESR) support RA or infection; uric acid tests assist gout diagnosis. - **Bone Scan or CT** — Used when tumors or avascular necrosis are suspected, especially in recurrent effusion cases. “No single test tells the whole story—pattern recognition across clinical history, exam, and lab results is key,” emphasizes Dr.
Rajiv Mehta, an orthopedic rheumatologist.
Treatment Pathways: From Conservative Care to Surgical Intervention
Treatment strategy hinges on etiology, severity, and patient factors such as age and activity level. The range spans conservative measures to advanced surgical options when needed.Conservative Management: First-Line Response
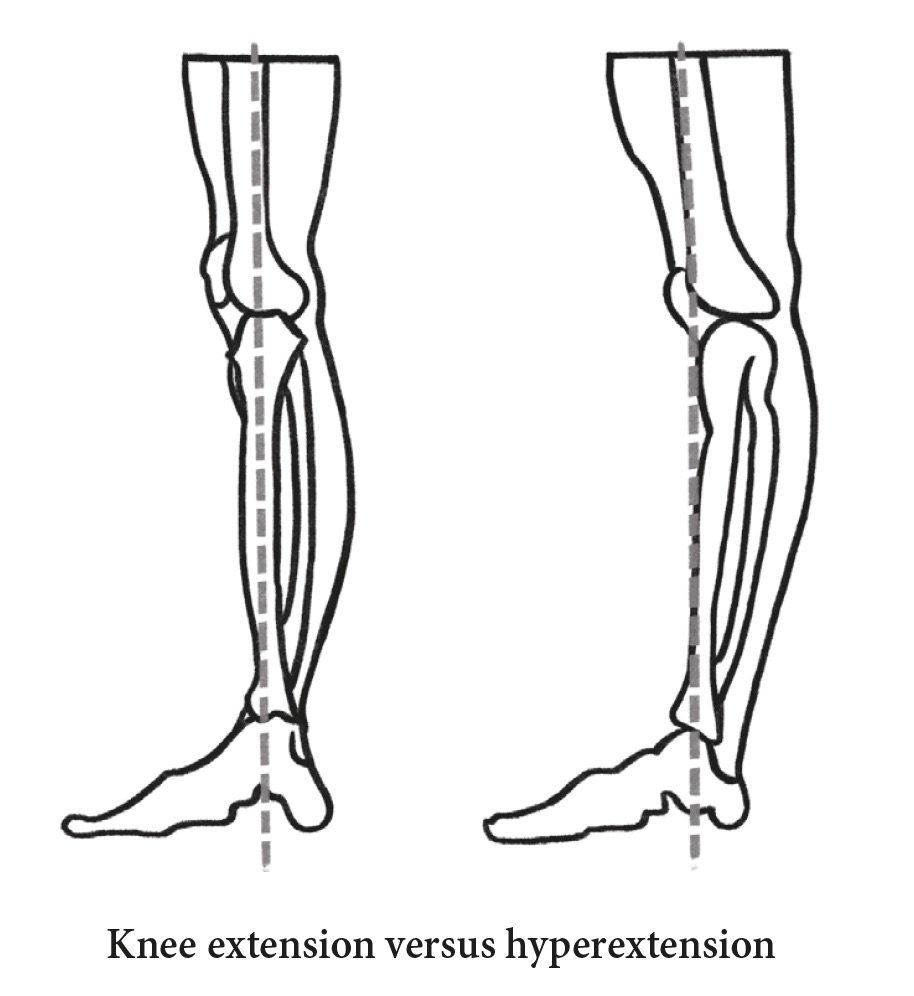
For mild effusions linked to mild injury, OA flare-ups, or early inflammatory conditions, non-invasive approaches often suffice: - Rest and activity modification reduce repetitive stress. - Physical therapy strengthens surrounding muscles—quadriceps and hamstrings support joint stability. - NSAIDs and intra-articular corticosteroid injections curb inflammation and fluid proliferation.Hyaluronic acid injections may improve joint lubrication. - Bracing or orthotics redistribute mechanical load, especially in alignment issues like genu valgum. - Weight management eases knee burden; even 5–10 pounds loss reduces stress by up to 40%.
Advanced Interventions for Refractory Cases
When conservative efforts falter or structural damage occurs, interventions escalate: - Arthroscopic surgery removes damaged tissue, loose bodies, or reparative synovectomy to quiet inflammation. - Hyaluronic acid injection improves joint mechanics and reduces pain in OA. - For end-stage wear or failed conservative therapy, total knee arthroplasty (TKA) offers durable relief—restoring mobility and function with modern implants.- In postoperative effusions, sinusoidal artery embolization or biologic therapies may address recurrent fluid accumulation.
Emerging and Alternative Approaches
Innovations under investigation include platelet-rich plasma (PRP), stem cell injections, and targeted biologics that modulate inflammatory pathways. Though not yet standard, these hold promise for future personalized care.The Integral Role of Patient Engagement and Long-Term Monitoring
Effective management extends beyond clinical intervention. Patients benefit from education on joint protection, exercise adherence, and early symptom tracking. Ongoing monitoring—via imaging and clinical follow-up—ensures timely adjustments to prevent recurrence.Lifestyle factors such as diet, hydration, and cardiovascular health influence synovial fluid dynamics, reinforcing a holistic approach to knee wellness. Understanding fluid buildup in the knee is no longer a matter of passive observation—it’s a proactive journey toward joint preservation. By decoding triggers, recognizing warning signs, and embracing timely, evidence-based treatments, individuals regain control over their mobility and quality of life.
In an era of advanced diagnostics and minimally invasive techniques, fluid accumulation need not define a life of limitation, but rather signal a clear path toward recovery and resilience.



Related Post

Decoding Mercedes Benz P0000: Unlocking the Code for Spark Plug Cluster Insights

Unraveling Schwartz-Jampel Syndrome: The Distinctive Symptoms That Define This Rare Movement Disorder

Understanding Septic Shock: The Deadly Cascade When Infection Overwhelms the Body

Osgood-Schlatter Disease: Unraveling the Pain Structure Behind Growing Pain in Young Athletes

