Unlock Access: How Utahns Can Quickly Check and Apply for Medicaid
Unlock Access: How Utahns Can Quickly Check and Apply for Medicaid
Navigating the path to healthcare coverage in Utah has never been more straightforward — if you know where to start. The Utah Medicaid Check Your Eligibility And Apply process is designed to be user-friendly, empowering residents to confirm coverage quickly and submit applications without unnecessary bureaucracy. With consistent updates to eligibility guidelines and streamlined digital tools, accessing Medicaid has become accessible to millions who need care.
Connecting with Utah’s Medicaid system means beginning with a simple, no-cost determination of eligibility — a critical first step that opens doors to comprehensive medical services, prescription support, and preventive care. “Checking eligibility takes minutes, but opens a lifetime of health security,” reports the Utah Department of Health and Human Services. Leveraging real-time data, the system ensures accuracy and speed, eliminating long waits or outdated paperwork that once deterred vulnerable populations.
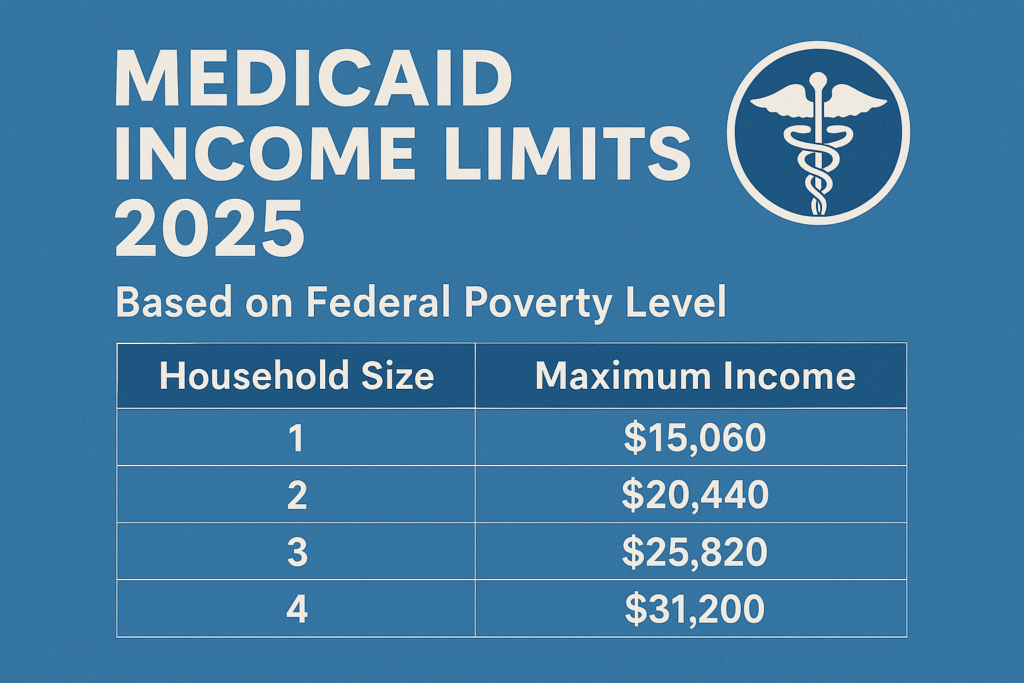
Utah’s Medicaid program, formally known as Utah Health Care Program (UHC), serves low-income families, pregnant women, children, seniors, and individuals with disabilities. Eligibility hinges on household income, household size, and specific life circumstances—factors now assessed through an intuitive online portal. The system automatically considers income thresholds updated annually, reflecting Utah’s cost of living and regional economic trends.
This dynamic assessment ensures fairness and responsiveness, adjusting benefits to match real financial conditions.
Checking eligibility begins with a few simple steps: visit the official Utah Medicaid website or use the state’s step-by-step eligibility calculator. Users input household income, residency status, and member demographics such as age, maternal status, or disability. Within seconds, the tool delivers a clear, personalized assessment — confirming whether income falls within qualifying range.
How the Eligibility Check Works: Precision in a Click
The Utah Medicaid eligibility verification process is built on transparency and speed.Once active, the system cross-references your information against federal and state databases, including income reports from tax records and utility filings. No need to collect or forward paperwork — updates are processed automatically in real time. This digital-first approach drastically reduces delays, allowing applicants to receive results that are both accurate and timely.
- Instant feedback within minutes - No upfront fees or hidden costs - Multilingual support available online - Accessible via desktop or smartphone - Real-time income validation against updated thresholds Each eligibility determination includes a clear factor breakdown — showing how income levels relate to expansion thresholds under the Affordable Care Act. For example, as of 2024, a family of four earning up to $42,000 annually qualifies, a figure adjusted annually to reflect inflation and local housing costs. This dynamic linking ensures coverage remains relevant and inclusive.
Applying Online: From Check to Coverage in Days
Once eligibility is confirmed, the next step is submitting a full application — an action now completed entirely online with minimal friction. Utah’s digital application platform is optimized for speed and clarity, guiding users through every required field with contextual help. Unlike past systems that demanded extensive form-filling and repeated document scans, today’s portal integrates secure upload functionality, enabling users to send identification, proof of residency, and other documents directly from their devices.Application speed is a hallmark of the modern Utah Medicaid process. Submitted applications trigger immediate processing, with initial confirmation emailed within 48 hours. Approval timelines average 21 business days, though expedited processing may apply for families with children, disabled members, or those facing acute health needs.
This timely turnaround ensures that qualifying individuals begin receiving benefits — including coverage for doctor visits, prescriptions, and preventive screenings — as soon as possible. The form collects essential details: household composition, primary residence, disability status, and employment history. Regional variables may influence required documentation—for example, rural applicants may receive tailored guidance on submitting alternate forms of identification due to limited physical office access.
Nonetheless, the entire workflow remains intuitive, with progress trackers and automated reminders guiding applicants through each stage.
After submission, beneficiaries benefit from a full suite of healthcare services. Importantly, Utah’s Medicaid expansion under the ACA ensures all eligible residents gain access to preventive care, maternity services, mental health supports, and chronic disease management — all at little or no direct cost.
This comprehensive framework reflects a commitment to equity, acknowledging that healthcare is not a privilege but a right supported by accessible systems.
Targeted Support: Who Should Apply — and Why
Medicaid eligibility in Utah is not based solely on income; it responds to life circumstances. Commonly eligible groups include:Children under 19 showing consistent low income
Pregnant women and new mothers in transitional housing
Seniors nearing retirement or already on fixed incomes
Disabled individuals meeting documented need thresholds
Families in foster care or facing homelessness
Even those with modest earnings — especially within families earning just above the self-cost threshold — may qualify. The program’s focus on fairness means that “small incomes” are not penalized; instead, eligibility hinges on overall household need, not individual thresholds.This inclusive model recognizes that financial stability is often a family matter, not an isolated condition.
Born from a broader vision of health equity, Utah’s Medicaid system now incorporates outreach strategies to reach underserved populations. Mobile application kiosks, community health center support, and multilingual outreach teams help ensure no eligible person is left behind.
“We’re not just checking eligibility — we’re connecting people to care,” says a Medicaid outreach coordinator. “Every eligibility check is a chance to transform health outcomes.”
The Truth Behind Wait Times and Assistance
Contrary to outdated perceptions, modern Utah Medicaid services eliminate prolonged helplessness. While initial application reviews are undergoing processing, the operational reality is lean: digitization reduces administrative backlog, and state funds support dedicated staff trained to handle inquiries efficiently.For those requiring physical documentation, Utah Health Care Program partners with local libraries, food banks, and social service centers to offer on-site assistance — turning administrative hurdles into manageable steps. Real-world examples reinforce the system’s effectiveness. Take the case of Maria Lopez, a single mother in Salt Lake County: “I didn’t think I qualified, until I used the online check.
Within 24 hours, the system confirmed eligibility. Now I’m insured for my son’s asthma medication and dental visits — services that mean everything.” Such stories illustrate the tangible impact of Utah’s efficient, user-first approach.
Navigating Common Challenges and FAQs
Even with a streamlined process, applicants may encounter occasional friction.Common questions include:
Can eligibility change? Yes. Income fluctuations, family size changes, or housing transitions may prompt re-evaluation. Updates are processed automatically when reported.
Do I need a Social Security Number? Required for identity verification; alternatives accepted if documentation is limited, with support from application counselors.
What if I’m uninsured but doesn’t count? Yes — Medicaid covers countless groups excluded from private plans, including low-income parents and people with disabilities who otherwise fall through coverage gaps.
Is there a cost to apply or maintain coverage? Not after eligibility is confirmed.
Premium waivers apply automatically, and no recurring fees are imposed during enrollment.
The system also integrates with federal and state databases, flagging potential fraud through secure validation, but sparing applicants from invasive checks. Transparency about data use builds trust — personal details are protected under Utah and federal privacy laws, accessible only to authorized personnel.Final Thoughts: Empowerment Through Access
Utah’s Medicaid Check Your Eligibility And Apply framework exemplifies how technology and compassion can converge to improve public health.By removing complexity, minimizing delays, and centering user experience, the state has transformed access from a daunting challenge into a straightforward right. For residents weighing healthcare options, the message is clear: navigate the steps, verify eligibility promptly, and apply without delay. The results are not just paper approvals — they are lifelines to consistent, affordable care for families, seniors, and individuals across every corner of the state.
In an era where healthcare access defines quality of life, Utah stands out as a model of efficiency and inclusivity — one where checking eligibility is no longer a barrier, but a bridge to wellness.

Related Post

Shotski The Ultimate Guide to the Meaning and Fun Behind the Iconic Moment

Como Se Dice Hola En Inglés: La Guía Definitiva Para Un Saludo Universal
King Von’s Autopsy Report Exposes Details Behind a Life Cut Short

Teen Titans RP on Roblox 2025: A Next-Gen Immersive Experience That Redefines Fan Engagement

