Unlocking Radicul O: The Silent Neurologic Clue in Back Pain Diagnosis
Unlocking Radicul O: The Silent Neurologic Clue in Back Pain Diagnosis
Radicul O, a clinical shorthand describing the compression or irritation of a nerve root within the spinal canal, represents a pivotal yet often overlooked factor in diagnosing and treating chronic back pain, radiculopathy, and referred neurological symptoms. While broadly understood in medical circles, its nuanced role in patient care remains underexplored by general audiences. This article delves into the anatomy, diagnostic challenges, treatment pathways, and real-world implications of Radicul O, revealing why precision in identifying nerve root involvement can dramatically alter patient outcomes.
The Anatomy of Nerve Root Compression: What Is Radicul O?
The term Radicul O stems from the Latin "radiculā," meaning root, and "O," symbolizing obstruction—specifically the compression of a spinal nerve root as it exits the intervertebral foramen. Each nerve root emerges from the spinal cord, snake-like through neural foramina, and carries both motor and sensory signals to specific body regions. When herniated discs, bony spurs, or spinal stenosis constrict these roots, nerve dysfunction ensues—manifesting as pain, numbness, tingling, or muscle weakness along the nerve’s distribution.Key Anatomy: - **Spinal Foramen:** The bony channel through which nerve roots exit the spinal column. - **Vertebral Foramina:** Smaller openings formed by adjacent vertebrae. - **Neuroforaminal Interface:** The junction where nerve roots pass through foramina and are vulnerable to compression.
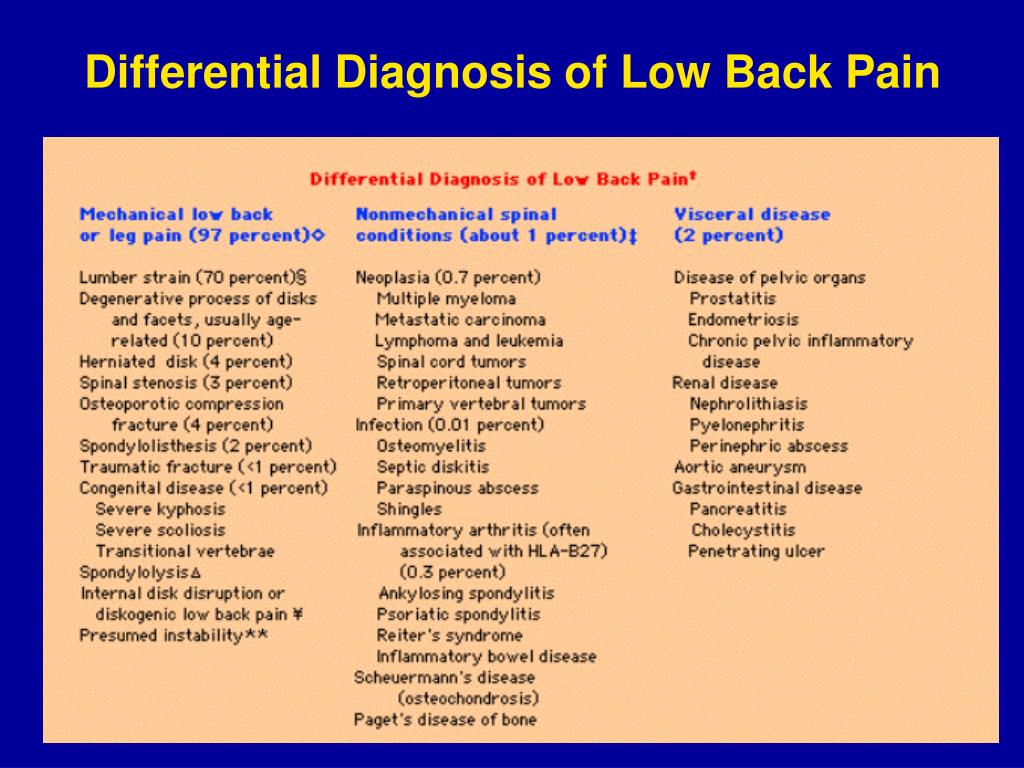
- **Common Sites of Compression:** Lumbar spine (L4–L5, L5–S1) and cervical spine (C5–C6) are frequent culprits, but Thoracic radiculopathies also occur. 《Nerve root compression disrupts the normal flow of impulses, transforming a simple backache into a complex neurological presentation that demands targeted intervention. Radicul O is not just a label—it’s a directive for clinicians to investigate with precision.
Diagnosing Radicul O: Challenges and Clinical Tools
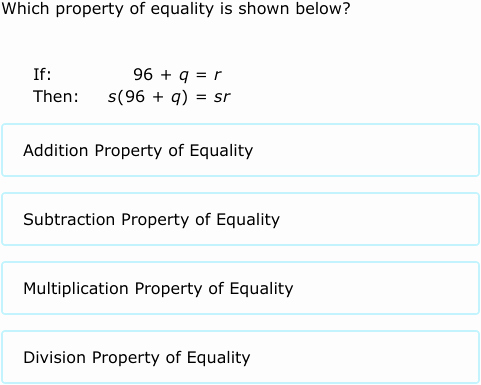
Accurately diagnosing Radicul O hinges on differentiating nerve root involvement from non-radiculopathy causes such as myofascial pain or peripheral neuropathy.Misdiagnosis remains a critical issue, with studies estimating up to 30% of patients with radicular symptoms incorrectly categorized. Clinicians rely on a multi-modal diagnostic approach: - **Patient History:** Localized pain radiating to a limb, worsened by movement or specific maneuvers (e.g., straight leg raise test), points to radicular pathology. - **Neurological Examination:** Reflex changes, muscle strength deficits, and sensory loss patterns help localize the affected root.
- **Imaging Modalities:** - MRI remains the gold standard, providing clear visualization of soft tissues, intervertebral discs, and spinal stenosis. - CT myelography offers high-resolution detail when MRI is contraindicated. - Plain X-rays detect bony anomalies but lack soft tissue sensitivity.
What makes Radicul O particularly diagnostic challenges is its overlapping symptomatology with non-radicular conditions. For example, a patient presenting with sciatica might have either disc herniation compressing the L5 root or a degenerative disc disease affecting a different level—each requiring distinct therapeutic pathways. Clinical Criteria for Radiculopathy Include: - Unilateral sensory loss or paresthesia along a dermatome - Muscle weakness in specific innervation zones (e.g., foot drop from L5 involvement) - Positive adapted straight leg raise test - Electromyography (EMG) confirming denervation in target muscles Bridging the gap between symptom presentation and definitive diagnosis is essential; delays in identifying Radicul O can lead to progressive neurological damage and diminished treatment efficacy.
Treatment Pathways: From conservative care to surgical intervention
Management of Radicul O is hierarchical, prioritizing non-invasive strategies before considering invasive options. The choice hinges on symptom severity, chronicity, and patient-specific factors such as age, comorbidities, and functional status. First-Line Therapies: - **Conservative Management:** - NSAIDs and muscle relaxants reduce inflammation and pain.- Physical therapy strengthens core stabilizers and improves mobility. - Epidural steroid injections deliver anti-inflammatory relief directly to compressed nerves, often providing symptom relief for weeks or months. - **Lifestyle Adjustments:** Ergonomic optimization, posture correction, and activity modification minimize mechanical stress on affected spinal segments.
When Interventional Options Are Warranted: - Failure of conservative care beyond 6–8 weeks. - Persistent or progressive neurological deficits. - Severe radicular pain unresponsive to medication.
- Structural instability or large disc herniation with neurologic compromise. Surgical decompression—such as microdiscectomy or laminectomy—remains reserved for cases involving spinal instability, recurrent herniation, or refractory radiculopathy. Minimally invasive techniques now offer faster recovery and reduced morbidity, though patient selection remains critical.
A pivotal World Health Organization report notes that 70–80% of patients experience substantial improvement with conservative care, underscoring the importance of early, accurate diagnosis to avoid unnecessary interventions. 《Radicul O is not merely a descriptor—it’s a clinical catalyst. Proper identification enables tailored treatment, preserves neurological function, and empowers patients to reclaim mobility and quality of life.
Living with Radicul O: Patient Empowerment and Prognosis
For patients navigating Radicul O, understanding the condition is as vital as medical treatment.Chronic back pain coupled with radicular symptoms often triggers anxiety and functional decline, yet proactive self-management significantly improves outcomes. Effective self-care includes: - Regular engagement in supervised physical therapy to maintain spinal flexibility. - Mindfulness and stress-reduction practices to mitigate pain perception.
- Consistent medical follow-up to monitor progress and adjust treatment. Long-term prognosis depends largely on early, appropriate intervention. Early-stage radiculopathy often responds robustly to conservative care, with most patients regaining full function within 3–6 months.
Delayed treatment, conversely, increases risk of permanent nerve damage and reduced treatment responsiveness. Real-world experience reveals that multidisciplinary care—integrating neurology, physical therapy, and pain management—yields the best results. Patient education programs focusing on anatomical literacy and symptom recognition empower individuals to make informed decisions and actively participate in their recovery.
In sum, Radicul O embodies the intersection of precise diagnosis and targeted care. By decoding this term, both providers and patients gain a clear lens through which to view one of spine medicine’s most influential mechanisms—transforming chesters of discomfort into pathways of healing.

Related Post

Is Rider AI a Powerful Time-Saver or Just Another Text Tool?

<strong>Master CA++ Validity Testing with SPSS & R: The Alief Akhman Formula That Simplifies Puja Cahaya dan SPSS Analysis</strong>
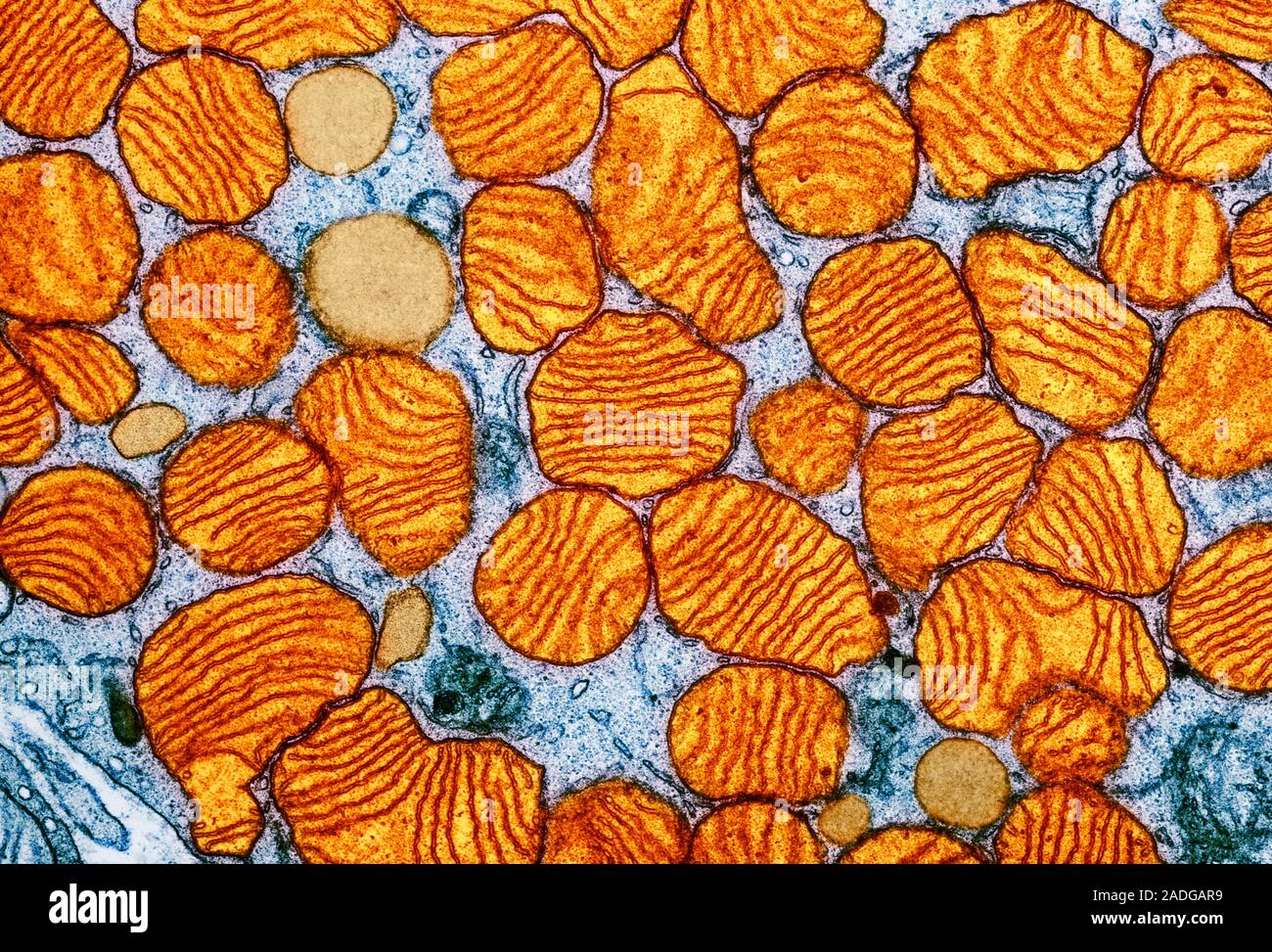
What Color Are Mitochondria? The Hidden Engineers of Light, Energy, and Life

Ring Realness Meets Real Power: The Dominance of WWE 2K on Switch