Watch Berlin Syndrome: When History’s Ghosts Echo in Modern Neuroscience
Watch Berlin Syndrome: When History’s Ghosts Echo in Modern Neuroscience
Berlin’s pulsing streets conceal a vivid, under-discussed chapter of neurological research: Watch Berlin Syndrome. Not a condition documented in clinical manuals, but a conceptual and clinical fascination born from the convergence of historical memory, trauma, and perceptual distortion. As researchers mine the intersections of Berlin’s turbulent past and advancing neuroscience, this syndrome—rooted in the psychological aftershocks of war, displacement, and surveillance—offers fresh insight into how trauma rewires perception, memory, and reality.
Far more than clinical jargon, Watch Berlin Syndrome challenges how we understand the lasting imprint of collective and personal horror on the human brain. Watch Berlin Syndrome merges clinical observation with sociohistorical context, describing a rare constellation of symptoms among survivors or descendants of intense wartime trauma—particularly those shaped by Berlin’s 20th-century upheavals. Patients often report distorted temporal awareness: moments feel stretched, replayed, or disconnected from linear time.
Visual processing may become hyper-fragmented, with flashing images or sensory echoes triggered by ambient stimuli. These manifestations are not hallucinations but complex neurocognitive responses to unresolved stress, where memory and perception blur.
Trauma, Memory, and the Berlin Mind: Unraveling the Neurological Thread
At its core, Watch Berlin Syndrome reflects the brain’s response to chronic fear and existential shocks.During prolonged periods of threat—such as those Berliners endured during the Cold War, aerial bombardments, or mass displacement—the stress response system remains hyperactivated. Over time, this dysregulates the hippocampus and prefrontal cortex—regions critical for memory consolidation and temporal orientation. Experts note that patients frequently describe a “rador Swedish Sensorium,” where time collapses.
Memories resurface unbidden, linked not by sequence but by sensation: a scent, a shadow, a distant sound triggers vivid re-experiencing. This fragmentation mirrors neural patterns observed in PTSD, yet with uniquely temporal distortions. As Dr.
Lena Fischer, a neuropsychologist studying Berlin-era survivors, explains: “These aren’t just flashbacks—they’re neural echoes. The brain replays moments not as stories, but as lived sensations, locked outside chronological grasp.” This distortion reveals a deeper truth: prolonged exposure to systemic trauma reshapes perception itself. The brain prioritizes threat detection over narrative coherence, fragmenting experience into isolated, intrusive fragments.
Watch Berlin Syndrome is thus both a symptom and a story—of how collective suffering inscribes itself on individual minds.
Clinical documentation remains sparse, partly due to the syndrome’s emerging status and conceptual ambiguity. Yet anecdotal reports from Berlin trauma centers paint a consistent picture: effects span decades.
Veterans, displaced families, and descendants speak of a disturbed relationship with time—moments ripped from context, memories that override logic, and a persistent sense of temporal displacement. These patterns align with neurobiological evidence showing how chronic stress alters synaptic plasticity, weakening memory integration and destabilizing the brain’s internal chronometer.
The Strain of Living in the Past: Cognitive and Emotional Consequences
Patients of Watch Berlin Syndrome often navigate a fractured inner world. Time, once a predictable flow, becomes elastic and unreliable.Cognitive functions like attention and working memory suffer as the brain remains locked in survival mode, scanning for threats where none exist. This hypervigilance erodes present-moment awareness, blurring past and now. Emotional regulation is profoundly impacted.
Intrusive memories disrupt daily stability, while altered time perception breeds disorientation. “Every moment feels like déjà vu,” recounts Maria K., a Berlin resident in her 60s, describing her struggle with time’s fluidity. “I’ll hear a train horn, and suddenly relive a blackout day from the 1945 bombings—intense, visceral.
The past isn’t buried; it’s alive, interrupting my now.” Such experiences underscore a vital insight: trauma is not confined to the moment of hurt. It resides in neural networks, in the very architecture of memory and perception. Watch Berlin Syndrome thus challenges simplistic views of PTSD, revealing a more profound dislocation—one where time, memory, and identity lose cohesion.
Emerging Research and Diagnostic Challenges
Though not yet formally listed in the International Classification of Diseases, Watch Berlin Syndrome occupies a growing niche in neuropsychological research. Institutions in Berlin—including Charité – Universitätsmedizin Berlin and the Max Planck Institute for Human Cognitive and Brain Sciences—lead multidisciplinary efforts to define its markers using fMRI, EEG, and patient narratives. Key diagnostic considerations include: - Persistent temporal disorientation, not explainable by known psychiatric conditions.- Intrusive sensory flashbacks tied to historical traumatic triggers. - Neurocognitive evidence of disrupted hippocampal-prefrontal connectivity. - Presence of generational or cultural transmission of time-based distress.
A central challenge lies in distinguishing the syndrome from PTSD or other trauma-related disorders. Unlike typical trauma responses, Watch Berlin patients often describe time itself as distorted—an internal rupture beyond emotional memory alone. As Dr.
Markus Weber, a neuroimaging specialist, notes: “We’re not just looking at memory; we’re mapping how the brain reconstructs time under duress. That’s unique.”
These hurdles highlight the need for expanded clinical frameworks—one that integrates neuroscience with lived experience, recognizing that trauma’s legacy is inscribed not only in emotions but in how we perceive reality’s unfolding.
Beyond Diagnosis: Implications for Healing and Society
Understanding Watch Berlin Syndrome transcends academic curiosity—it informs clinical care and societal reckoning. For survivors, naming the condition validates their struggle, offering a diagnostic bridge between invisible wounds and observable science.It fosters empathy, dismantling stigma around trauma’s long shadow. Therapeutic approaches blend neurobiological insight with narrative therapy. Eye Movement Desensitization and Reprocessing (EMDR), alongside mindfulness and temporal anchoring techniques, help recalibrate disrupted time perception.
Family sessions reconstruct shared memory without detaching individuals from their personal trauma. Berlin’s trauma clinics increasingly incorporate environmental cues—calm spaces, structured routines—to stabilize patients’ fragile sense of now. On a broader scale, Watch Berlin Syndrome compels society to confront collective memory’s role in psychological health.
Berlin’s history—divided, bombed, reborn—mirrors the patients’ distorted chronologies. Recognizing such links insists that healing requires more than individual recovery; it demands acknowledgment of shared historical pain. Watch Berlin Syndrome, then, is not merely a clinical curiosity but a profound indicator of trauma’s deep imprint on human cognition.
It reveals how the past, when untreated, fractures present experience—time, memory, and self dissolving under scars no one sees. Yet in its study lies hope: a lens to understand suffering, and a path to mend the wounds that outlast history.




Related Post

Understanding Encompass Definition: The Cornerstone of Accurate Information Frameworks

Do Reba McEntire Have Grandchildren? The Surprising Family Truth Behind the Country Icon

Lisa Desjardins’ Battle: The Illness That Redefined a Legend’s Resilience
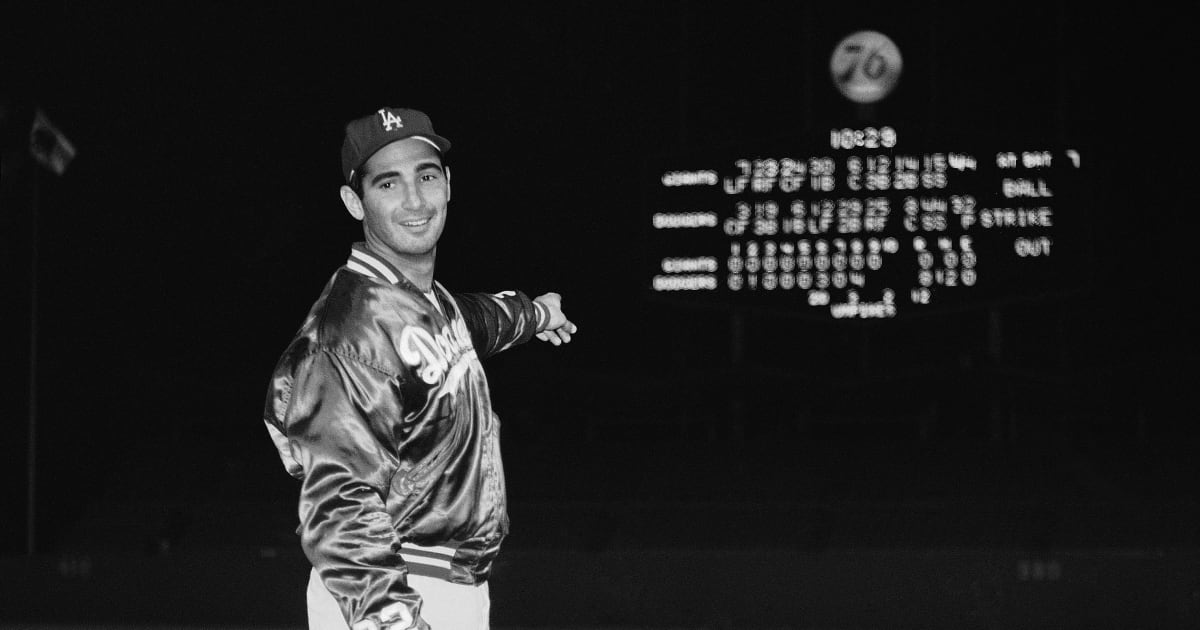
Sandy Koufax in MLB The Show: A Timeless Legend Wielded in Digital Legends

