What Is A Concordance Rate? Understanding This Critical Measure in Healthcare and Research
What Is A Concordance Rate? Understanding This Critical Measure in Healthcare and Research
Concordance rate stands as a vital statistical indicator in clinical trials, diagnostic testing, and epidemiological research—quantifying the degree to which test results or prognostic predictions align across practitioners, methodologies, or over time. Far more than a mere number, the concordance rate reflects reliability, consistency, and trust in medical assessments. It answers a fundamental question: how often do two different evaluators or two test methods yield the same outcome when applied to the same set of cases?
With growing demands for precision medicine and reproducible results, understanding concordance has never been more urgent—and its implications stretch from individual patient care to global public health strategy.
Defining Concordance Rate: Precision in Medical Evaluation
At its core, the concordance rate measures agreement between two or more evaluation standards or healthcare providers. Typically expressed as a percentage, it denotes the proportion of cases in which the results or predictions from different assessments coincide.For diagnostic tests, this means how frequently a test correctly matches the clinical diagnosis across multiple observers. For predictive models in risk assessment, it reflects consistency in forecasting patient outcomes. In clinical contexts, a high concordance rate—often targeting 90% or above—is seen as a hallmark of robust, reliable tools.
For example, a gold-standard imaging scan that matches a specialist’s interpretation in 95% of cases demonstrates strong diagnostic concordance. In contrast, low concordance may signal ambiguity, bias, or systematic error that undermines confidence in clinical judgment or test validity. How Concordance Rate Is Calculated Calculating concordance rate follows a structured statistical framework.
When testing diagnostic accuracy, the classic approach involves a 2×2 contingency table, categorizing subjects based on agreement (concordant) or disagreement (discordant) between two methods or raters. The formula commonly used is: Concordance Rate = (Number of concordant pairs) / (Total number of comparisons) × 100 In more advanced models—such as the Kappa statistic or sensitivity-specificity matrices—concordance accounts for both true agreement and chance agreement, providing a nuanced measure less susceptible to sampling bias. According to epidemiologist Dr.
Julian Mercer, “Concordance isn’t just about whether two opinions match—it’s about quantifying how much that match reflects a true, stable pattern, not random coincidence.”
Applications Across Medicine and Research
The utility of concordance rate spans multiple domains. In cancer screening, it helps determine how reliably radiologists or pathologists identify malignancies. Studies evaluating mammography and biopsy results regularly report concordance rates to judge whether imaging findings consistently indicate true tumor presence.In mental health, clinicians use concordance to assess inter-rater reliability in diagnosing conditions like depression, where subjective symptom reporting plays a major role. Diagnostic Testing In diagnostic testing, concordance rate directly influences test adoption and clinical policy. For instance, rapid antigen tests for infectious diseases like influenza or COVID-19 are assessed not only by sensitivity and specificity but also by how consistently they align with polymerase chain reaction (PCR) gold standards across labs.
High concordance reinforces confidence in field testing rapidity versus lab accuracy. Predictive Modeling Beyond diagnosis, concordance is crucial in predictive analytics. In oncology, tools designed to forecast recurrence risk must demonstrate strong concordance with actual patient outcomes.
Hospitals and research consortia increasingly require high concordance values before deploying algorithms for treatment planning, ensuring model predictions are actionable and patient-safe.
Between 80% and 95% concordance rates are often considered excellent in clinical validation studies, though benchmarks vary by context. For example, electrocardiogram interpretations may achieve 98% concordance among experts, while self-reported pain scales in community settings might register at 65–75%, reflecting inherent subjectivity.
Factors Influencing Concordance Rates
Numerous variables shape concordance, from technical settings to human behavior. Key contributors include: - **Tester expertise and training**: The experience and certification level of clinicians significantly impact agreement. - **Measurement variability**: Differences in equipment, calibration, or protocol can skew results.- **Case complexity**: Ambiguous or borderline cases challenge even the most accurate methods, increasing discordance. - **Timing of assessments**: Laboratory tests conducted at different times may yield variable outcomes due to biological fluctuations. Human Bias and Systemic Challenges Even with standardized procedures, cognitive bias—such as anchoring, confirmation bias, or availability heuristics—can distort diagnostic judgment.
Studies cited by the American College of Physicians reveal that two experienced doctors may disagree on 15–20% of complex cases due to interpretive differences. Systematic efforts such as consensus conferences, double-blind reviews, and AI-assisted decision support aim to reduce these discrepancies.
Real-World Examples: Concordance in Action
Consider recent trials in stroke risk prediction using machine learning.A 2023 multicenter study found a concordance rate of 89% between AI-driven risk scores and expert clinical assessments—marking a leap toward reliable automation in preventive cardiology. Conversely, in prenatal screening, some non-invasive DNA tests showed concordance levels as low as 78%, prompting updated guidelines emphasizing confirmatory invasive testing. In dermatology, dermoscopy evaluation combined with clinician assessment achieves concordance rates exceeding 90% for melanoma detection—demonstrating how complementary approaches enhance diagnostic reliability.
These examples underscore that while concordance rates vary, they remain a cornerstone in validating clinical tools and fostering trust in medical decision-making.
The Future of Concordance in a Data-Driven Era
As precision medicine and digital health evolve, the role of concordance rate grows more sophisticated. Integration with artificial intelligence demands new standards for measuring cross-platform agreement across algorithms trained on diverse datasets.Emerging techniques like probabilistic concordance modeling and mixture approaches promise deeper insights into situational reliability—helping clinicians and researchers navigate uncertainty with greater clarity. Ultimately, concordance rate is not merely a statistical metric but a gateway to trustworthy care. It bridges the gap between subjective assessment and objective truth, ensuring that medical tools and expert opinions converge reliably.
In an age where data fuels decision-making, understanding and optimizing concordance remains essential—for patients, providers, and the future of healthcare itself.




Related Post

Mt125 Loose Gear: Unmasking the Hidden Causes of Drivetrain Complaints

Did Ben Mankiewicz Leave TCM? What We Know This Season
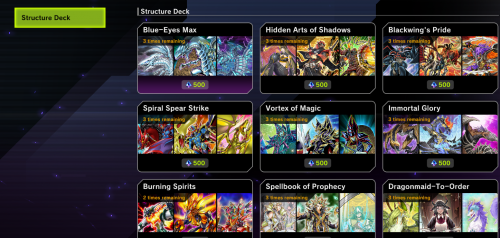
Yu-Gi-Oh! Master Duel: The Ultimate Structure Deck Tier List & Rankings for the Modern Strategist

Saiki Kū’s Dual Legacies: English Dub vs. Japanese Cast—Unpacking Two Powerful Versions of a Cult Icon

