Yearning for Clarity: The Long Road to Diagnosing Lower Left Rib Cage Pain
Yearning for Clarity: The Long Road to Diagnosing Lower Left Rib Cage Pain
For years, a persistent ache in the lower left rib cage gnawed silently at my well-being—often dismissed as muscle strain or acid reflux. What began as an occasional discomfort evolved over time into a constant, unsettling presence, distorting both daily life and sleep. The pain was stifficuous to pin down—sharp one moment, dull and aching the next—often accompanied by subtle pressure, occasional sharp twinges, and heightened sensitivity on deep breaths or deep pressure.
Decades of self-diagnosis, scratchy medical appointments, and countless misleading suggestions delayed the revelation of a complex, underlying issue rooted not in muscles or the diaphragm, but in intricate visceral and neurological pathways. Understanding this pain demands more than symptom journaling—it requires a meticulous dissection of subtle bodily signals eventually uncovered through persistence, advanced diagnostics, and targeted treatment.
The lower left rib cage is a region of surgical anatomical nuance, housing not only ribs and chest wall muscles but also critical organs: the spleen, parts of the stomach and colon, peripheral nerves, and lymphatic structures.
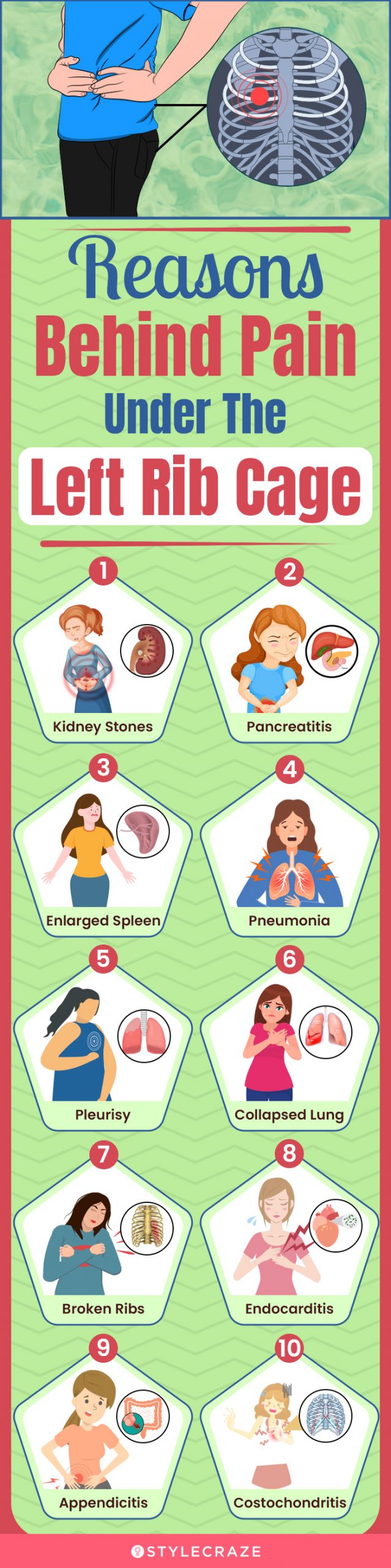
Yet its proximity to the diaphragm creates a convergence zone for sensory signals from both visceral and somatic origins, making differential diagnosis particularly challenging. Patients often describe the sensation as a burning discomfort masked by overlapping cues—eye of vincula in medical terms, where internal pain is misinterpreted by pain perception pathways as rib-floor irritation. The journey to uncover the true source began with exhaustive exclusion: ruling out common causes like costochondritis, rib fractures, and gastrointestinal indigestion with no definitive match.
Symptom Complexity: Why Lower Left Rib Pain Confounds Diagnosis
The primary challenge in diagnosing pain in the lower left rib cage lies in its symptom overlap with numerous conditions—from acute musculoskeletal strain to life-threatening pathologies. Key features frequently reported include:- Location: Pain localized beneath the left ribs, sometimes radiating to the flank, flank, or abdomen—distinguishing it from central or upper chest pain.
- Quality and Variability: A mixture of burning, pressure-like, and sharp, intermittent pain worsened by deep lung expansion or pressure on the abdomen.
- Triggering and Alleviating Factors: Deep breathing exacerbates discomfort; relief comes intermittently with rest or avoidance of heavy meals and strenuous exertion.
- Associated Signs: Subtle gastrointestinal disturbances such as bloating, nausea, or altered bowel habits often accompany the pain, blurring the line between visceral and somatic origins.
These tools revealed that the root cause was not nociception originating in the ribi itself, but a misfiring signal pathway linking epithelial irritation in the distal colon to the somatic nociceptors of the left rib cage.
What followed was a recalibration of diagnostic focus: identifying the “referred” pain phenomenon, where inflammation or inflammation-mediated neuropathic signaling from internal organs activates peripheral nerve terminals near the ribs, creating the illusion of structural damage at the bony perimeter. In my case, subtle low-grade inflammation and microtrauma within the splenic hilum—compounded by connective tissue sensitivity—acted as a persistent nociceptive trigger, amplifying sensory feedback to the rib cage’s sensory nerves.
The body’s alarm system had misfired, interpreting internal biochemical distress as mechanical injury—a phenomenon neurologically rooted in viscerosomatic convergence.
Diagnostic Breakthrough: Mapping the Hidden Trigger
The diagnostic breakthrough emerged through advanced imaging and functional neurological mapping, revealing that the lower left rib region was responding to signals far removed from the bony structure. Key findings included:Treatment Strategy: From Diagnosis to Targeted Relief
Once the multifaceted cause was identified, treatment shifted from symptomatic management to addressing root mechanisms. Initial phases involved:The journey from persistent, misunderstood lower left rib cage pain to definitive diagnosis and treatment reveals the critical importance of clinical vigilance, interdisciplinary insight, and patient-driven persistence. What began as an vexing, enigmatic symptom evolved into a profound lesson in how internal stress ripples outward, manifested not in organs alone, but in every nerve, muscle, and breath. Understanding this pain demands more than imaging—it calls for empathy, sustained inquiry, and a willingness to navigate the labyrinth where gut, nerve, and bone converge.
With accurate diagnosis and tailored care, relief is not a distant hope, but a tangible reality.



Related Post

Shiba Inu Updates and Spaces: Where Community, Innovation, and Canine Culture Collide

The Multifaceted Genius of Donald Glover Sr: Beyond the Screen, a Tapestry of Talent

Roxy After Dark Comic

Exploring 9xmoovi: Your Ultimate Guide to Streaming Movies Online with Unmatched Ease and Quality

