American Trypanosomiasis Treatment
In the shadow of tropical diseases lurking beyond remote villages and isolated borders, American Trypanosomiasis Treatment stands as a critical frontier in combating a neglected yet deadly parasitic threat. Caused primarily by parasites of the genus *Trypanosoma*, this disease — particularly Chagas disease — affects millions across the Americas, transmitted through insect vectors and often latent for years before symptoms emerge. While historically overshadowed by more prevalent global health challenges, recent advances and persistent efforts are reshaping the landscape of treatment and prevention.
This article explores the current state of American Trypanosomiasis treatment, the drugs transforming care, enduring obstacles, and what the future holds for patients and public health.
The Silent Killer: Understanding Chagas Disease and Its Impact
Chagas disease, also known as American trypanosomiasis, is caused by *Trypanosoma cruzi*, a parasite spread mainly by triatomine bugs, commonly called “kissing bugs.” Though rarely transmitted through blood donations or congenitally, its silent progression over decades makes it a formidable public health issue. The World Health Organization estimates over 6 million people currently live with active infection, mostly in rural Mexico, Central America, and part of South America. Left untreated, it damages the heart and digestive system, leading to chronically disabling conditions such as heart failure or megacolon.“Because symptoms often don’t appear for years, many go undiagnosed until irreversible damage occurs,” notes Dr. Elena Marquez, infectious disease specialist at the Centers for Disease Control and Prevention. “By the time traditional chronic signs appear—like an enlarged heart or jagged esophagus—it’s often too late for simple interventions.” p American Trypanosomiasis Treatment centers on early detection and targeted antiparasitic drugs.
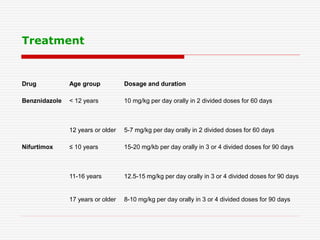
Two main classes dominate clinical use: benznidazole and nifurtimox. **Benznidazole and Nifurtimox: Core Therapeutic Agents** Benznidazole, a nitrostatin derivative, remains the frontline chemotherapy for acute and congenital Chagas infection. Administered in daily doses over 60–90 days, it disrupts *T.
cruzi’s* ability to replicate and invade host cells. Nifurtimox, a related compound, offers an alternative with similar efficacy but a more complex dosing schedule and higher risk of side effects, limiting its routine use. Both drugs target the parasite at different growth stages, making combination or sequential regimens an area of active research.
“Benznidazole’s success hinges on timely initiation,” explains Dr. Marquez. “When given early, it achieves cure rates exceeding 70% in children and 50–60% in adults—limitations shaped by access, compliance, and toxicity.”
Clinical trials continually refine dosing, duration, and patient selection.
Longer treatment periods with close monitoring improve outcomes, yet side effects—ranging from mild rashes and nausea to neurological disturbances—remain a challenge. For chronic cases, where drug penetrates tissues poorly, alternatives or adjunctive therapy are explored, though no definitive cure exists yet outside intensive regimens.
Barriers to Effective Treatment: Access, Awareness, and Neglect
Despite effective drugs, treatment coverage for Chagas disease remains alarmingly low. Chronic infections persist in populations with limited healthcare access, poverty, and geographic isolation.Diagnosing early infection requires sensitive serological tests, which are underutilized in endemic regions due to cost and infrastructure gaps. “We see delayed diagnosis particularly among migrant populations,” states Dr. Marquez.
“Many arrive later in disease progression, compounding management difficulties.” Additional challenges include drug availability, variability in national health policies, and insufficient surveillance systems. While the U.S. maintains strict blood screening and newborn testing in endemic zones, many Latin American countries lack standardized protocols.
“Global neglect has left Chagas in the shadows,” observes Dr. Carlos Rivera, a tropical medicine researcher at the Pan American Health Organization. “Until treatment becomes rapidly accessible and prevention more robust, the fatality burden will continue rising.”
Another critical hurdle is drug resistance and pharmacokinetics.
No large-scale resistance has been documented to benznidazole in standard use, but suboptimal absorption in malnourished or pediatric patients reduces efficacy. Research into extended-release formulations and targeted delivery is underway to overcome these barriers.
Innovations on the Horizon: New Drugs, Diagnostics, and Prevention Strategies
Progress is accelerating in the fight against American Trypanosomiasis. Preclinical studies and early-phase trials are exploring novel antiparasitics with improved safety profiles and broader tissue penetration.Compounds targeting *T. cruzi*’s unique metabolic pathways offer promise for chronic phases, where current drugs falter. Point-of-care diagnostics are also emerging, enabling rapid field testing with high sensitivity.
These tools, coupled with mobile health messaging in remote communities, aim to shorten time-to-diagnosis and treatment initiation. “Long-acting injectable formulations could revolutionize care,” says Dr. Rivera.
“Imagine a single dose curing active infection—this is no longer science fiction.” Vector control remains foundational. Public health campaigns promoting bed nets, insecticide spraying, and housing improvements reduce triatomine exposure. Community education on avoiding bug habitats further disrupts transmission cycles.
“Impactful prevention requires integrating Chagas control into broader tropical disease programs,” notes Dr. Marquez. “Early detection in newborns, screening blood donors, and treating infected vectors collectively turn the tide.” Collaborative efforts between U.S.
and Latin American institutions are strengthening research networks, clinical trials, and policy advocacy, fostering a more coordinated response.
Understanding transmission routes is essential. Unlike Lyme disease, Chagas transmission centers on specific ecological niches—rural homes with thatched roofs, rural work environments, and unsafe blood products.
“This specificity means targeted interventions yield high returns,” explains Dr. Marquez. “Uniting vector control with medical treatment creates a dual shield against spread.”
Global health leaders stress the need for sustained investment.
Chagas disease exemplifies the neglected tropical diseases category—effective treatments exist, yet underfunding and low political priority stall progress. “Innovations save lives, but only when paired with equitable access,” urges Dr. Rivera.
“Nothing short of a global commitment can break the cycle.” The landscape of American Trypanosomiasis treatment is evolving, marked by scientific rigor, persistent challenges, and emerging hope. With effective drugs like benznidazole forming the backbone of care, new tools on the horizon promise more durable cures. Yet, overcoming barriers of access, awareness, and healthcare infrastructure remains paramount.
As research deepens and global partnerships strengthen, the vision of eliminating unnecessary suffering from Chagas disease draws nearer—but only through collective commitment can treatment become universal, and disease obsolete.

Related Post
Navigating the Fight Against African Sleeping Sickness: Current Treatment Options and Realistic Patient Expectations

Marianne Bachmeier: The Infamous Video That Shocked the World

Mapping the Harvest: How Agricultural Density Shapes Human Settlements

Mha Fantasy Au Unveiled: The Mythical Realm Crafted for Epic Immersion

