Utah Medicaid: Transforming Access to Care in the Mountain State
Utah Medicaid: Transforming Access to Care in the Mountain State
In a state where vast, rugged landscapes meet pockets of economic strain, Utah Medicaid has emerged as a vital lifeline, expanding healthcare access to tens of thousands of low-income residents. Since its expansion under the Affordable Care Act, the program has evolved into more than just a health insurance option—it’s a comprehensive safety net reshaping how Vulnerable populations navigate medical care. With over 780,000 Utahns now enrolled—more than a 40% increase since 2014—Utah Medicaid is not only improving health outcomes but also setting a model for efficient, equitable public health policy in the American West.
The scale of Utah’s Medicaid expansion speaks to its impact. In 2014, just over 130,000 Utahns lacked health coverage, but by 2023, more than three times that number—some 780,000 individuals—were enrolled, covering essential primary care, mental health services, prescription medications, and chronic disease management. This surge reflects a deliberate policy shift toward inclusion, with outreach campaigns, simplified enrollment through the Single Source for Service portal, and trusted community navigators helping residents overcome administrative barriers.
What distinguishes Utah Medicaid from many regional programs is its integration of care coordination and preventive services. “We’re not just paying claims—we’re investing in long-term health,” explains Dr. Karen Fisher, Director of Health Equity at the Utah Department of Health and Human Services.
“Our providers receive incentives for reducing hospital readmissions and keeping patients engaged in preventive screenings—ducts closed, YCDs delivered, lives extended.” This proactive model has reduced preventable ER visits by 18% in just three years, according to state health data. The Medicaid expansion also prioritized behavioral health, a growing concern across the nation. In Utah, over 40% of Medicaid enrollees now access mental health and substance use disorder services, with telehealth options significantly expanding reach—especially in rural communities like the Uinta Basin and Sanpete Valley, where providers were historically scarce.
“Telehealth became a real equalizer,” says Maria Gonzalez, a behavioral health specialist in St. George. “Patients who once drove four hours for care now connect from home.
That’s access, plain and simple.” Financing Utah’s expansion relies on a carefully balanced funding structure. The state contributes upfront through state lotteries, federal matching funds, and rehabilitation trusts, while federal dollars cover the largest share—largely through block grants under Section 1915(c) of the Social Security Act. “Utah’s strategy is fiscally disciplined but forward-looking,” notes Robin Wells, a health policy analyst at Brigham Young University.
“We reinvest savings from reduced uncompensated care into program sustainability and outreach—ensuring Medicaid doesn’t grow at the expense of taxpayer burden.” Impact on health outcomes is measurable. In counties with robust Medicaid uptake, infant mortality rates have declined by 12%, diabetes management has improved, and late-stage cancer diagnoses have dropped by nearly 20%, aligning more closely with national benchmarks. For children, vaccination rates hit 94%, surpassing the U.S.
average of 91%, while prenatal care utilization surged to 87%—a critical factor in reducing maternal mortality. Critically, Utah Medicaid’s administrative efficiency has drawn national attention. Automated eligibility checks, synchronized data systems across hospitals and clinics, and streamlined appeals processes mean smoother enrollment and faster access.
“We’re not perfect, but we’re relentless,” says Chef Manuel, a Spanish-speaking patient in Salt Lake City who enrolled 18 months ago after being turned away once due to paperwork. “They helped me get in on my first try. That’s not just service—that’s dignity.” Challenges remain, especially in scaling behavioral health capacity and addressing persistent rural-urban disparities in specialist access.
Yet Utah continues to innovate—piloting mobile clinics in gaming towns, expanding school-based health centers, and leveraging artificial intelligence to predict coverage gaps before enrollment closes. What makes Utah Medicaid a case study in success? It combines political will with policy precision, warmth of care with data-driven accountability.
“This isn’t about who gets insurance,” says Fisher. “It’s about guaranteeing no one in Utah faces a medical crisis without support. That’s how real equity looks.” As the state looks ahead, Austin D.
Smith, chair of the Medicaid Medicaid Policy Commission, emphasizes sustainability. “We’re not static—we’re evolving. Our goal is a system where every Utahn knowing Medicaid means care not just when illness strikes, but when wellness flourishes.” In Utah, Medicaid has grown from a safety net into a pillar of community resilience—a testament to what policy change can achieve when design meets purpose.
Utah’s Medicaid expansion illustrates how strategic public investment in health care can transform lives across diverse landscapes. By prioritizing access, integration, and innovation, the program not only increases insurance rates but also drives tangible decreases in preventable illness and mortality. As one local provider observes, “When people get consistent care, everything changes—families stabilize, schools thrive, and communities grow steadier.” This model, rooted in data and compassion, demonstrates that Medicaid isn’t just a program.
It’s a promise fulfilled.


Related Post
Unlock Access: How Utahns Can Quickly Check and Apply for Medicaid
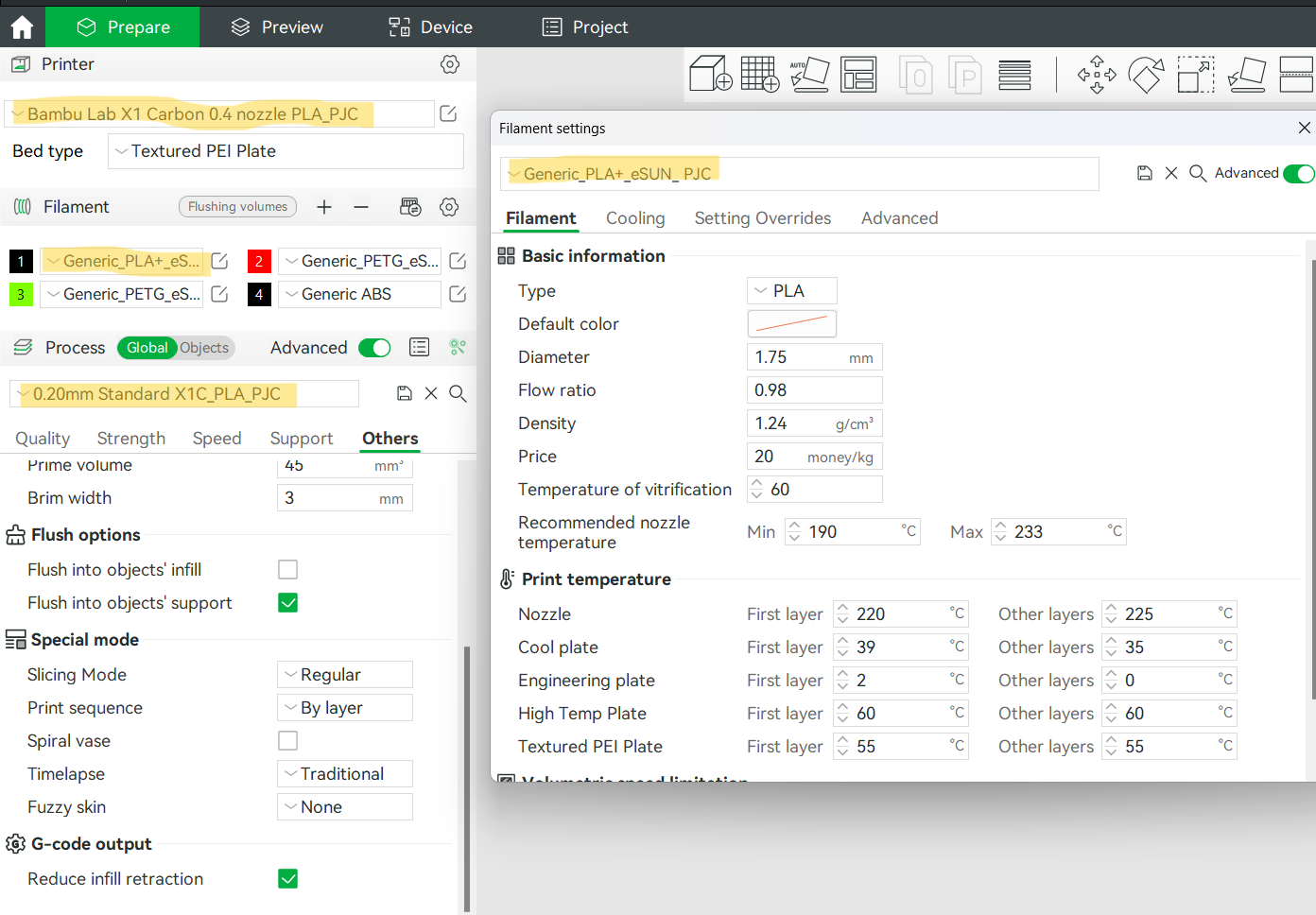
Unlock Faster 3D Printing: Mastering Speed Settings in Bambu Lab Studio
Decoding Dfkm: The Internet Acronym Reshaping Digital Culture
Winning Eleven Brasileirão PS1: A Nostalgic Dive into Brazil’s First Rhythm-Driven Soccer Simulator

